May 22, 2023
One of the most rewarding diagnoses that I make is a simple cataract. Whether the patient is 50 or 90 years old, knowing that a simple, out-patient procedure will provide them with a lifetime of vision is a wonderful feeling. Knowing that I will be the quarterback of the team providing this care is awesome as well. We have all participated in cataract management to some degree or another, and as such, all of us know how excellent our patient’s vision is after cataract surgery. However, many of us are unaware of an extra benefit that cataract surgery provides — it lowers intraocular pressure.
The extent and duration of this phenomenon was analyzed by Stephen Mansberger in a seminal article published in Ophthalmology, Sep 2012, 119(9).1 The author studied a cohort of patients who were enrolled in the Ocular Hypertension Treatment Study (OHTS).
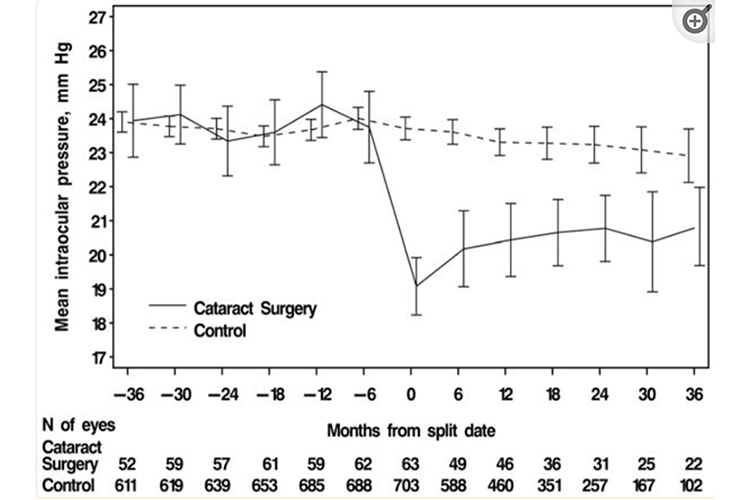
All the patients in this sub-analysis had ocular hypertension, defined in this study as between 24 mm Hg and 32 mm Hg. The fellow eye could have IOP as low as 21 mm Hg. This was a multi-centered study in which all the subjects had multiple IOP readings taken. None of the patients in this analysis were on a topical medication for the IOP nor had they ever received a glaucoma laser treatment. The subjects were divided into two arms; those who underwent cataract surgery and those who did not. The question asked was whether cataract extraction lowered IOP in comparison to those who remained phakic, and if so, for how long did this effect last?
IOP in Surgical Group Decreased
The stratification of the two groups pre-analysis was similar. The pachymetry readings for the surgical group was 584 microns as compared to 571 microns in the no surgery group. The cup-to-disc ratios were 0.39/0.39 in the surgical arm and 0.36/0.39 in the non-surgical arm. The surgical patients were a bit older, averaging 64.1 years, whereas the no surgery patients averaged 55 years old. IOP before any surgery was similar at 23.9 mm Hg among the surgical patients, compared to 23.8 mm in the no surgery group. The results were rather eye-opening! (Pardon the bad pun.)
The IOP in the surgical group decreased to an average of 19.8 mm Hg, whereas the IOP in the non-surgical arm remained essentially unchanged at 23.9 mm Hg. Moreover, this 16.5% decrease in IOP lasted for the extent of the study, which was three years. The simple act of cataract surgery resulted in a 4 mm reduction in intraocular pressure with no other glaucoma surgery adjunctive procedure.
A few other notable findings occurred as well. For example, 39.7% of the surgical patients recorded post-operative IOP > 20% below their pre-operative IOP. Also, those patients who had higher IOP pre-operatively experienced a greater percentage of IOP reduction after the surgery than those with lower pre-operative IOP. Furthermore, the IOP-lowering effect was more pronounced in patients who had narrower angles pre-operatively than in those who had grade 3 angles or wider. Though that would not be unexpected, it was certainly borne out in the analysis of the data.
The authors did not speculate on a mechanism as to why this phenomenon occurred. Perhaps it is the simple deepening of the angle after cataract extraction that allowed the IOP to be reduced or perhaps the ultrasonic waves of a phacoemulsification procedure are actually therapeutic to the trabecular meshwork. Other thoughts have been bandied about around this, but no clear mechanism of action for this effect was proposed by the authors.
Lasting Impact of IOP Reduction Debated
A decade later, Dr. Mansberger, as part of the OHTS study group, looked at the same group of patients to analyze whether the data remained the same at 48 and 72 months. The results of this study were published in the American Journal of Ophthalmology 2 in 2022. Interestingly, this showed that the IOP difference between the two groups become statistically nonsignificant after 36 months. Causing some to point out that this IOP reduction does not last long enough to provide any real benefit to the long-term outcome for glaucoma patients. However, if you look closely at that data you will see that there are indeed long-term positive effects for these patients. For instance, 23% of these patients remained free of needing any topical medication for reducing IOP, and 41% had a reduced medication. This reduced medication burden was sustained for 72 months.
So, how should we look at this data as clinicians? First, accept the easy answer that removing a patient’s cataract is beneficial to their IOP. Though the initial IOP reduction may only last for three years, that bridge time is certainly beneficial as it delays the need to use IOP-lowering drops. Additionally, remember that 23% of these patients remained drop free without any other surgery for 72 months. There is true patient benefit for both of those scenarios. We know clearly that the less drops a patient needs and the shorter time they need said drops, the better their compliance.
Another fact that should not be overlooked is that over 40% of these patients need fewer glaucoma medications than those who did not have cataract surgery. That leads to fewer side effects and better compliance, not to mention a cost savings to that patient. Although you cannot make this conclusion from this study, a doctor can certainly surmise that this phenomenon occurs in patients who do not have elevated intraocular pressure, and this may indeed be protective to the optic nerve in those patients.
I am not saying that there is not a role for MIGS procedures such as iStent or trabectomes for ocular hypertensive patients with cataracts. Those procedures are extremely safe and effective. But, armed with this data, a doctor can now have a more educated discussion with their ocular hypertensive patient around whether an additional procedure is needed at the time of cataract surgery. Not all patients desire an additional procedure, and for those who don’t or for patients you’ve determined do not need it, this data should make you feel better about going down the cataract extraction only route.
References
1 Mansberger, et. al. Reduction in intraocular pressure after cataract extraction: the Ocular Hypertension Treatment Study. Ophthalmology. 2012 Sep;119(9); 1826-1831
2 Mansberger, et. al. Cataract Surgery Lowers Intraocular Pressure and Medication Use in the Medication Group of the Ocular Hypertension Treatment Study. Am J Ophthalmol. 2022; 236; 53-62