April 11, 2023
Demodex is a microscopic parasite that lives in and near hair follicles. The prevalence of demodex on the skin is common, with reports of it affecting in the range of 40-50% of adults around age 50.1 There are over 65 species of demodex, but only two, demodex brevis and demodex folliculorum, live on humans and are responsible for demodex blepharitis (DB).2
Although underdiagnosed, DB is very common.3 A retrospective study of over 1,000 patients showed a prevalence of DB in 57% of U.S. eye care patients.3 The same study also showed that only 44% of patients with collarettes, the pathognomonic sign for demodex, had been diagnosed with DB. Given the high prevalence of DB, this presents an incredible opportunity to diagnose and thus better care for our patients.
Mechanism of Demodex Blepharitis
Demodex is resourceful and has multiple mechanisms. Mechanically, demodex mites attach to follicles and cause lash distension.4-5 Demodex mites deposit debris and digestive enzymes that cause additional eyelid margin irritation.5,6 Demodex mites have a bacterial component and contribute to DB by transporting bacteria on their exterior surface that may provoke immune responses.4,7-8 The chemical component of demodex is associated with altered meibum composition.9 Demodex mites debris may cause chronic inflammation and degeneration of conjunctival tissue.10
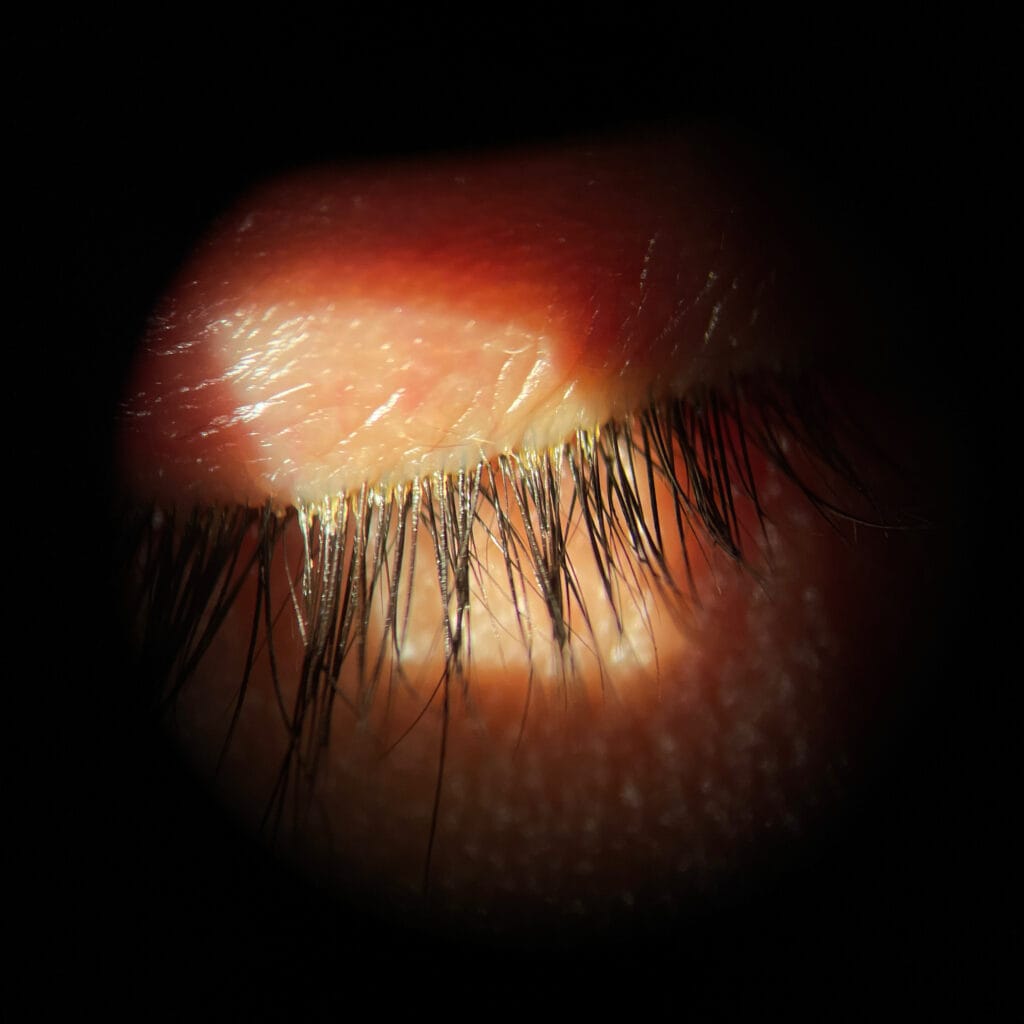
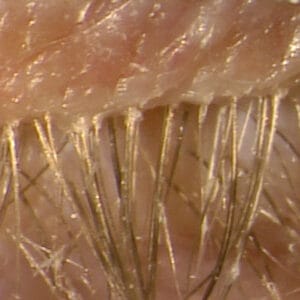
Signs of Demodex Blepharitis
Patients with DB can be asymptomatic, so a thorough evaluation of the patient’s lids and lashes is critical. The presence of collarettes, also known as cylindrical dandruff, at the base of the eyelashes are pathognomonic for DB. The debris is likely a combination of demodex digestive excretions and mite eggs.11 Other signs include lash madarosis, trichiasis, lid margin erythema, and meibomian gland dysfunction. Subjective symptoms of DB include itchy eyes, dry eyes, foreign body sensation, and tearing.12
Ocular Surface Disease and Demodex Blepharitis
There is extensive overlap between the signs and symptoms of DB and ocular surface diseases. An impaired tear film could make the environment more hospitable for demodex mites. When demodicosis is unrecognized or untreated, it can exacerbate ocular surface disease, causing severe symptoms.13 It has been demonstrated that individuals with DB have lower quality meibum14 with higher concentrations of (O-acyl)-ω-hydroxy fatty acids (OAHFAs) in their meibum,15 which may potentially exacerbate meibomian gland dysfunction, leading to tear film instability.
Treating Demodex Blepharitis
Existing management options for DB are inconvenient, burdensome, and may be ineffective and/or toxic to the ocular surface.
Tea tree oil, also known as melaleuca oil, is an essential oil thought to have antibacterial and anti-inflammatory properties. It comes from steaming the leaves of the Australian tea tree. Terpinen-4-ol(T40) is the most active ingredient of tea tree oil and has been found to be effective at killing demodex mites.16 However, more recent research shows that even a low concentration of T40 can be toxic to meibomian gland cells.17
In-office microblepharoexfoliation can be effective at removing collarettes from the base of the lash. In addition, intense pulsed light may be another useful treatment against demodex. The pigmented exoskeleton of the demodex mite absorbs the light energy, which causes their death.
The good news is that there is a promising topical treatment with the potential to significantly reduce or eliminate demodex mites and collarettes, which are the pathognomonic sign of demodex. In a recent multi-center, randomized, controlled study, lotilaner ophthalmic solution, 0.25%, (TP-03, Tarsus Pharmaceuticals, Irvine, CA, USA), demonstrated significant improvements in mite eradication, collarette elimination, and eyelid erythema reduction compared to the vehicle.18
It is important to recognize and treat DB due to its impact on the meibomian glands and the ocular surface. Smoldering inflammation from DB infestation can cause chalazion, hordeolum, meibomian gland dysfunction, and atrophy. Early recognition and treatment of DB will provide the best outcomes.
References
1 Foley R, Kelly P, Gatault S, Powell F. Demodex: a skin resident in man and his best friend. J Eur Acad Dermatol Venereol. 2021 Jan;35(1):62-72. doi: 10.1111/jdv.16461. Epub 2020 May 15. PMID: 32294279.
2 Rather PA, Hassan I. Human demodex mite: the versatile mite of dermatological importance. Indian J Dermatol. 2014 Jan;59(1):60-6. doi: 10.4103/0019-5154.123498. PMID: 24470662; PMCID: PMC3884930.
3 Trattler W, Karpecki P, Rapoport Y, Sadri E, Schachter S, Whitley WO, Yeu E. The Prevalence of Demodex Blepharitis in US Eye Care Clinic Patients as Determined by Collarettes: A Pathognomonic Sign. Clin Ophthalmol. 2022 Apr 15;16:1153-1164. doi: 10.2147/OPTH.S354692. PMID: 35449733; PMCID: PMC9017705.
4 Zhang AC, Muntz A, Wang MTM, Craig JP, Downie LE. Ocular Demodex: a systematic review of the clinical literature. Ophthalmic Physiol Opt. 2020 Jul;40(4):389-432. doi: 10.1111/opo.12691. Epub 2020 Jul 21. PMID: 32691894.
5 Liu J, Sheha H, Tseng SC. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010 Oct;10(5):505-10. doi: 10.1097/ACI.0b013e32833df9f4. PMID: 20689407; PMCID: PMC2946818.
6 Fromstein SR, Harthan JS, Patel J, et al. Demodex blepharitis: clinical perspectives. Clin Optom (Auckl). 2018 Jul 4;10:57-63. doi: 10.2147/OPTO.S142708. PMID: 30214343; PMCID: PMC6118860.
7 Gao YY, Di Pascuale MA, Li W, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci. 2005 Sep;46(9):3089-94. doi: 10.1167/iovs.05-0275. PMID: 16123406.
8 Zhu M, Cheng C, Yi H, et al. Quantitative Analysis of the Bacteria in Blepharitis With Demodex Infestation. Front Microbiol. 2018 Jul 31;9:1719. doi: 10.3389/fmicb.2018.01719. PMID: 30108572; PMCID: PMC6079233.
9 Li J, O’Reilly N, Sheha H, et al. Correlation between ocular Demodex infestation and serum immunoreactivity to Bacillus proteins in patients with Facial rosacea. Ophthalmology. 2010 May;117(5):870-877.e1. doi: 10.1016/j.ophtha.2009.09.057. Epub 2010 Jan 15. PMID: 20079929; PMCID: PMC2946826.
10 Gao H, Chen H, Xie HT, et al. Changes in Meibum Lipid Composition With Ocular Demodex Infestation. Transl Vis Sci Technol. 2021 Dec 1;10(14):6. doi: 10.1167/tvst.10.14.6. PMID: 34874449; PMCID: PMC8662575.
11 Tarkowski W, Moneta-Wielgoś J, Młocicki D. Demodex sp. as a Potential Cause of the Abandonment of Soft Contact Lenses by Their Existing Users. Biomed Res Int. 2015;2015:259109. doi: 10.1155/2015/259109. Epub 2015 Jul 21. PMID: 26290865; PMCID: PMC4523645.
12 Nicholls SG, Oakley CL, Tan A, Vote BJ. Demodex species in human ocular disease: new clinicopathological aspects. Int Ophthalmol. 2017 Feb;37(1):303-312. doi: 10.1007/s10792-016-0249-9. Epub 2016 May 9. PMID: 27160273.
13 Schachter S, Yeu E, Holdbrook MJ, et al. Clinical Manifestations of Demodex Blepharitis. Invest. Ophthalmol.Vis. Sci. 2021;62(8):1268.
14 Rabensteiner DF, Aminfar H, Boldin I, et al. Demodex mite infestation and its associations with tear film and ocular surface parameters in patients with ocular discomfort. Am J Ophthalmol. 2019;204:7-12.
15 Ziaja-Sołtys M, Kołodziejczyk M, Rymgayłło-Jankowska B, et al. Massive demodicosis of the eyes in a patient with Sjögren syndrome: A case report. Acta Parasitol 2021;66(2):677-681.
16 Tighe S, Gao YY, Tseng SC. Terpinen-4-ol is the Most Active Ingredient of Tea Tree Oil to Kill Demodex Mites. Transl Vis Sci Technol. 2013 Nov;2(7):2. doi: 10.1167/tvst.2.7.2. Epub 2013 Nov 13. PMID: 24349880; PMCID: PMC3860352.
17 Chen D, Wang J, Sullivan DA, et al. Effects of terpin-4-ol on meibomian gland epithelial cells in vitro [published online ahead of print September 16, 2020]. Cornea.
18 Yeu E, Wirta DL, Karpecki P, et al. Lotilaner ophthalmic solution, 0.25% for the treatment of Demodex blepharitis: Results of a prospective, randomized, vehicle-controlled, double-masked, pivotal trial (Saturn-1). Cornea. 2022; Online ahead of print.