April 11, 2023
Stop me if you’ve heard this one before. A man walks into an optometrist’s office complaining of blurry vision. After thoroughly examining the patient, the doctor informs him that he has a cataract. Shocked, the patient asks his doctor if this can be cured. She responds by saying, “The good news is that we can remove the cataract and greatly improve your vision. The bad news is that you have astigmatism…”
This may seem like an extreme overstatement, but look at the data. We have all embraced cataract surgery and its ability to enhance people’s vision. Yet doctors, both referring optometrists and the surgeons performing the surgery, are much more hesitant to recommend toric IOLs to correct pre-operative astigmatism. Surgical data show that a little more than one-third of all patients undergoing cataract surgery have >1.00D of astigmatism, which is the minimum amount necessary for a toric IOL. Yet only about 40% of those patients “eligible” for a toric IOL actually receive one. This is a mind-blowing statistic to me. What if you fit only 40% of your contact lens patients who had cylinder greater than 1.00D in toric CL? Imagine the disappointed patients (and the subsequent bad social media reviews)! I think that is a very fair way to view the recommendation of toric IOLs to your cataract patients. If their refraction would lend itself to toric contact lenses, then they would likely benefit from a toric IOL.
What About Astigmatism and Cataract Surgery?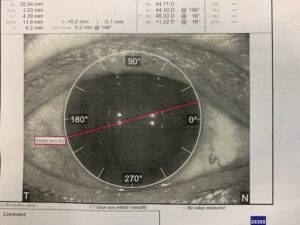
There are a few different means to correct this intra-operatively. Limbal relaxing incisions can, and are, still being used. This technique can realistically reduce corneal astigmatism up to 1.00D in the steep axis. It is less costly to the patient but less effective and predictable. Some surgeons opt to perform a laser-guided astigmatic keratotomy to reduce corneal astigmatism. Using a femtosecond laser, the surgeon can make up to three relaxing incisions at the limbal cornea. Each of these can reduce between 0.50D and 0.75D of corneal astigmatism. The surgical challenges are deciding where to put these incisions to correspond with the patient’s cylinder axis and the fact that these add time to the procedure.
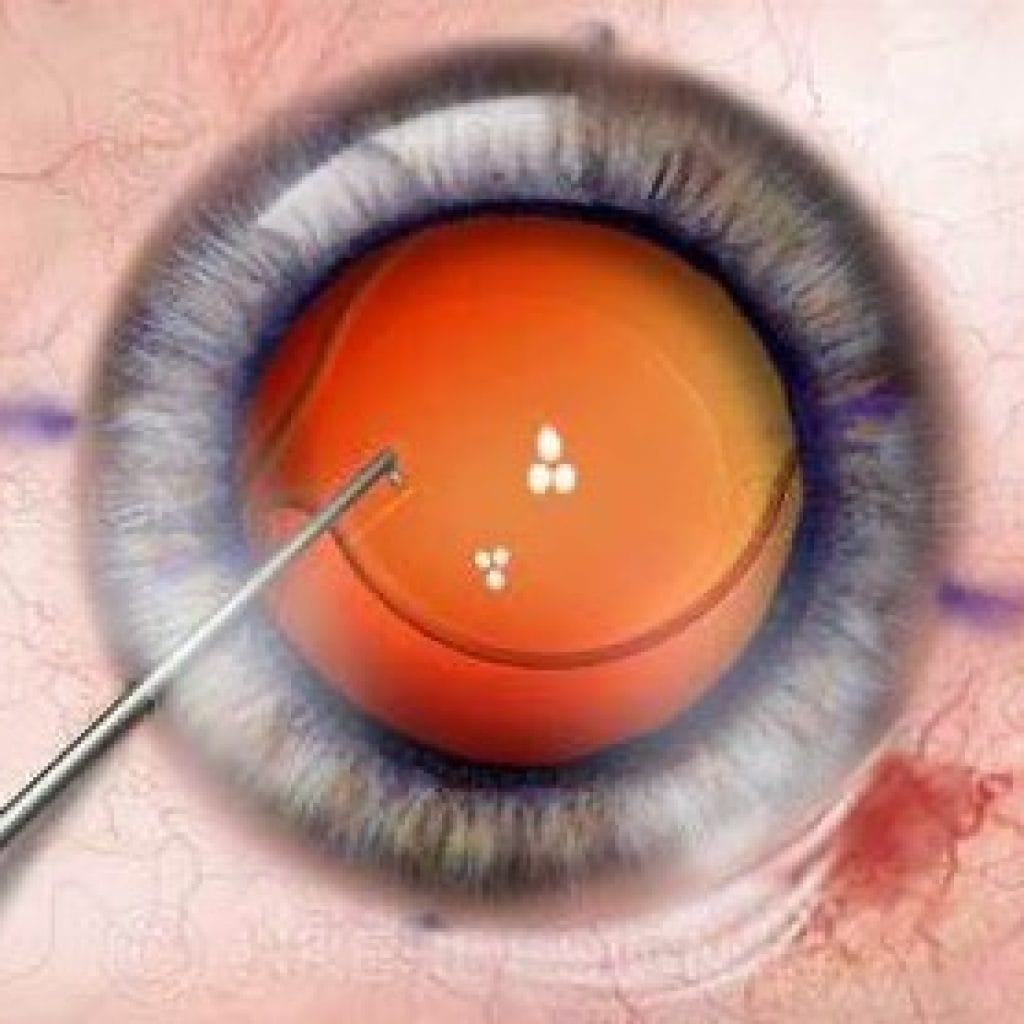
Toric IOLs are a far more predictable method of correcting or reducing pre-operative astigmatism. They can predictably correct up to 5.00D of corneal cylinder. There is very little additional surgical time required for implanting these. The biggest surgical challenge is simply aligning the axis of the toric IOL with the refractive axis of the patient’s corneal cylinder. This is achieved by marking the patient’s cornea at the steep axis and properly aligning the toric IOL with that corneal marking. Just as in carpentry, the old adage, “measure twice, cut once,” should be applied.
Toric IOLs, like toric contact lenses, have markings on them to indicate the axis. Depending on the IOL brand, that marking should be lined up at 3:00 and 9:00 axis, the 6:00 and 12:00 axis, or directly at the axis of the corneal cylinder of the individual patient. The remainder of the surgical procedure is exactly the same as using a standard monofocal IOL.
One caveat to remember when deciding whether to recommend a toric IOL or not is the fact that toric IOLs correct corneal astigmatism only. So, you must figure out how much of the patient’s refractive astigmatism is due to the cornea. That can be done by looking at the keratometric readings. Remember, the simple act of removing the cataract will eliminate any lenticular-induced astigmatism.
The Impact of Insurance on IOLs
Another factor to keep in mind, and likely the main reason why the uptake of toric IOLs is lagging, is that there is an upcharge for these IOLs. Most insurance will not reimburse for these IOLs. The surgery and implant will get reimbursed but at the same rate as a traditional monofocal implant. The upcharge is necessary because these IOLs are more costly to purchase, require additional surgical expertise, and post-operative care is a bit more time-consuming. The typical upcharge for a toric IOL surgery is about $1,500 per eye. This cost is borne directly by the patient and is generally shared by the surgeon and the co-managing optometrist. These charges should absolutely be discussed with the patient as you are discussing the need for surgery, just like you, the co-managing doctor, should be discussing the reasons why you are recommending a toric IOL. The initial discussion around a toric IOL and the reasons for the recommendation should absolutely begin with the referring doctor.
When you refer your patient for toric IOL surgery, it should be incumbent that you as the primary doctor should be rendering the post-operative care. The reimbursement for this comes from the 66984-55 code submitted to the proper insurance, but there is also your fee for management of the specialty toric IOL portion of the procedure. The basics of the post-op care are the same as any standard cataract surgery. These patients are generally on a combination of topical antibiotics, NSAIDs, and steroids as decided by you and the surgeon (and unfortunately the insurance company in many instances). But there is some delicacy to managing the toric IOL post-operatively, and this is where the additional upcharge comes into play.
Rotation Can Be a Complication
It is imperative to look for rotation of the IOL. This is best achieved through dilating the patient and should be done at the three-week post-op exam. The toric IOL will have marks, as described before. These markings need to be lined up to the desired axis. Rotation of these IOLs is the biggest complication, and if this occurs, the earlier it is noted and the earlier it can be rectified the better the outcome.
Fortunately, 94% of these procedures show rotational stability at six months, and the average rotation is 2.74 degrees. Any rotation less than 5 degrees is deemed to be acceptable. Assessing for rotation is a big deal. A recent study published in the Journal of Cataract and Refractive Surgery showed that a loss of 3.3% in cylindrical power occurs for every 1 degree of rotation away from the intended axis. To put this in subjective terms, a rotation of 10 degrees results in a 33% reduction of cylinder correction, which means that if you have a 2.25 cylinder, a 10-degree rotation will result in an actual cylindrical correction of 1.50D. This is a meaningful loss. This rotation stability needs to be assessed regularly for the first six months post-operatively. If this is seen, an immediate referral should be made to the surgeon, who can typically reposition the lens by rotating it. Rarely do these IOLs need to be explanted.
Embrace the toric IOL opportunities for your patients. Correcting astigmatism at the nodal point yields far crisper acuity than correcting it at the spectacle plan. Your patients will see better, and you will be rewarded with more and happier patients (as well as a little extra revenue).