April 11, 2023
Meibomian gland dysfunction (MGD) is present in 86% of dry eye patients, and effectively treating MGD requires addressing gland obstruction.1 There are multiple possible causes of MGD, some of which are intrinsic (such as aging 2), and others that are extrinsic (such as digital device use). All of these particularly affect the “Generation 45+” patient.
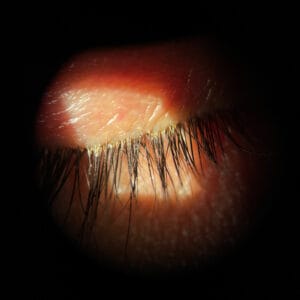
When addressing MGD, it is important to target both obstruction and inflammation. Factors that affect obstruction are hormonal therapy,3 congenital absence of meibomian glands, demodex,4 microbiological changes, contact lens wear,5 disruption of the lipid layer by medications and structure damage to the glands by cicatricial conditions. However, despite the cause of MGD, most all cases of MGD can be effectively managed by addressing obstruction.
Arita et al. proposed diagnostic criteria for obstructive MGD by comparing clinical findings between individuals with obstructive MGD and normal controls.5 The ocular symptom score, lid margin abnormality score, meiboscore, and SPK score were significantly higher in the obstructive MGD compared to the control group. When two out of three of the scores are abnormal, obstructive MGD should be suspected. When all three are abnormal, obstructive MGD is likely. Additionally, break up time was significantly shorter in the obstructive MGD group compared to the control group. This is helpful information, however clinically, simply pushing on the lids can illustrate if obstruction is present.
Tremendous Opportunity to Treat Patients with Meibomian Gland Dysfunction
Given how common MGD is in our aging dry eye patients, we need to have an effective way to treat this. In an ocular surface disease survey of optometrists and ophthalmologists published in 2021, 87% of participants responded that obstruction is a vital component of MGD, and 71% stated that obstruction removal should be the first-line treatment for patients with MGD, however, only 5% of patients received thermal expression treatment.6
Many providers recognize the importance of treating MGD, however, few are incorporating MGD treatment in practice. For effective evacuation of the glands, heat application along with evacuation of the glands is needed. Fortunately, we have multiple in-office devices to better treat obstructive MGD.
Some of the Thermal MGD Treatments Available
Lipiflow uses heat on the posterior surface of the eyelids while pressure is applied to the anterior surface of the lids. Lipiflow uses a 12-minute treatment using vector thermal pulsation. After the use of a numbing drop, dome-shaped, single-use activators are placed in the eye to provide heat to the meibomian glands. The heat in addition to pressure on the lids liquifies meibum and removes blockages.
TearCare is a portable device that uses localized heat to the upper and lower eyelids. A single-use SmartLid is applied to the patient’s eyelids and allows patients to blink during the treatment to facilitate meibum expression. The treatment provides 15 minutes of heat that melts the thick meibum and after, the doctor performs manual meibomian gland expression. The most recent clinical data showed the positive effects of TearCare lasted 12 months.7
Systane iLux2 is a portable handheld device that uses light-based localized heat and controlled compression therapy. The doctor is able to control the level of compression and can visualize the glands and meibum that is expressed during the treatment. It also has the ability to capture meibomian gland imaging as well as take video of the expression for patient education. The treatment takes 8-12 minutes.
The MiBo ThermoFlow supplies continuous controlled heat to the outer eyelid by utilizing a thermoelectric heat pump to augment liquefaction of meibum. Along with the controlled heat, MiBo ThermoFlow uses ultrasound gel for a gentle massage. The Elite Tip covers both upper and lower glands and uses movement to massage the eyes during treatment. The C-Elite Tip requires less movement during treatment, covers the entire ocular surface, and envelops the heat into the glands.
OptiLight Intense Pulsed Light (IPL) is the first and only FDA-approved IPL for the treatment of meibomian gland dysfunction. It is a light-based therapy that uses polychromatic light of varying wavelengths to cause targeted photothermolysis. It works by reducing the levels of proinflammatory mediators, destroys abnormal blood vessels which perpetuate inflammation, decreases demodex population, and improves meibomian gland morphology and function. There are usually a series of four treatments, spaced two to four weeks apart. Each treatment typically lasts 15 minutes. Expression may be done after IPL treatment.
Regardless of your preferred choice of expression, it’s critical to address obstruction to improve dry eye symptoms and prevent gland atrophy. In-office treatments can speed the symptom relief when warm compresses are not enough.
References
1 Lemp MA, Crews LA, Bron AJ, Foulks GN, Sullivan BD. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012 May;31(5):472-8. doi: 10.1097/ICO.0b013e318225415a. PMID: 22378109.
2 Obata H. Anatomy and histopathology of human meibomian gland. Cornea. 2002 Oct;21(7 Suppl):S70-4. doi: 10.1097/01.ico.0000263122.45898.09. PMID: 12484702.
3 Sullivan DA, Sullivan BD, Ullman MD, et al. Androgen influence on the meibomian gland. Invest Ophthalmol Vis Sci. 2000 Nov;41(12):3732-42. PMID: 11053270.
4 Gao H, Chen H, Xie HT, et al. Changes in Meibum Lipid Composition With Ocular Demodex Infestation. Transl Vis Sci Technol. 2021 Dec 1;10(14):6. doi: 10.1167/tvst.10.14.6. PMID: 34874449; PMCID: PMC8662575.
5 Arita R, Itoh K, Maeda S, et al. Proposed diagnostic criteria for obstructive meibomian gland dysfunction. Ophthalmology. 2009 Nov;116(11):2058-63.e1. doi: 10.1016/j.ophtha.2009.04.037. Epub 2009 Sep 10. PMID: 19744718.
6 Survey of optometrists and ophthalmologists conducted by PentaVision LLC, publishers of Optometric Management and Ophthalmology Management from October 7, 2020 through November 5, 2020, and January through April 2021, Data on file. 2. Market Scope 2021 Ocular Surface Disease Survey
7 https://mytearcare.com/clinical/