March 4, 2024
For every generation, there is the progression of change and the loss of simplicity. In our profession it is not so much that we are finding new diagnosis, rather we are finding easier ways to treat and diagnose the conditions that have been plaguing our patients for decades . . . no, make that centuries.
Today’s technological boom has created a sense of comfort, and yet, also a larger chasm of loss. What seems to be missing is the desire to do research and ask the questions that will elucidate a desired a response, which was required way back in the early 2000s. We didn’t just look at ocular coherence tomography (OCT) and play the game of red light, green light. When we diagnosed glaucoma, it was predicated on risk factors, checking IOPs (with Goldmann) diurnally, obtaining a visual field, photos, and then the patient discussion. James Burke and Robert Ornstein elucidated this point in their book The Axemaker’s Gift: A Double-Edged History of Human Culture. They stated that as societies develop more tools, enabling a faster, easier production of goods and services, we use less of the tool that got us to this point — our brain.
Still, as technology evolves, the hackneyed way of treating and diagnosing conditions should be in flux at all times. As our society ages, it seems that we have more advanced ways to enhance and cure the commonly encountered ophthalmic maladies. As someone who has been in the lanes for three decades it is not lost on me that as technology advances, we have to keep our approach to vision care at the same pace. Most notably for me when I manage patients for refractive opportunities I try to remove any obstacles to an ideal outcome.
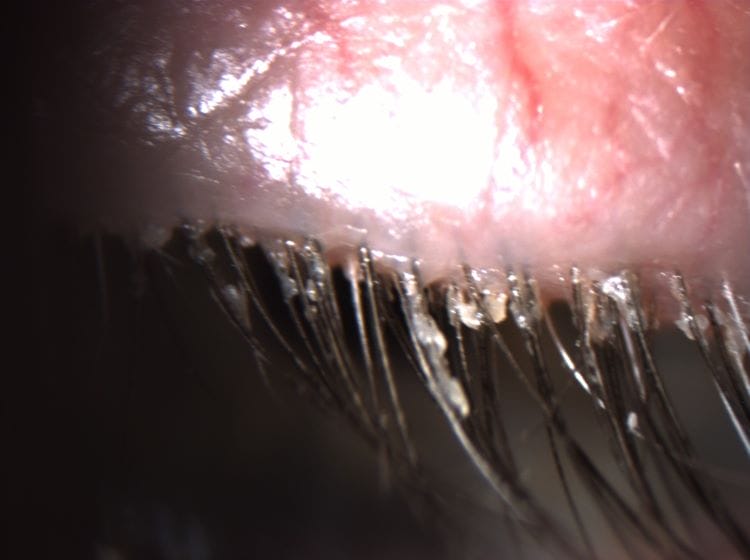
Take for example demodex blepharitis. Demodex is not a new diagnosis. We did not just wake up after years of slumber like Brendan Fraser in Encino Man (circa 1992) and say, “Oh look there must be eight-legged bugs in the follicles that are making this nastiness on the base of the lash, inducing redness, itching, and exacerbating dry eye.” Rather, we needed technology to provide us a treatment, like Xdemvy (lotilaner ophthalmic solution 0.25%) from Tarsus to eradicate the source, the demodex, so we can then manage the residual collarettes with lid wipes.
Demodex blepharitis on the surface may not seem that common. However, in a recent study it was diagnosed (via collarettes) in 58% of the population. (Trattler W, et al. Clin Ophthalmol. 2022;16:1153-1164. 2. O’Dell L, et al. Clin Ophthalmol. 2022;16:2979-2987.) In fact, of this subset of the population, 56% of these patients had cataracts. Furthermore, it was established that almost half were contact lens wearers.
The ability to eradicate these ectoparasites is a sea change for the pre-operative management of cataract and refractive surgeries. Since these eight-legged invaders carry unique bacteria (Bacillus oleronius), induce inflammation, and create micro-abrasions with their claws, it is in our best interest to manage the lids prior to surgery. Therefore, we now need to tell our patients, prior to any surgery (or contacts, or glasses), they have “mites” or as I like to say, “You have ectoparasites in your follicles that are living their best lives. Ask me how to kill them.”
A further example of this modernizing practice is the way we communicate about and manage cataracts now versus when I started practicing in the mid-1990s. Back in the boy band days of the ’90s, we waited until the patient was so hampered by the sclerosis of the lens that we actually gave it a diagnosis, cataract, and then lamented with our patients that they are now seniors, old, senile! As I have opined many a times prior, cataracts have never been an old-timer’s diagnosis. There has always been this progression of heating proteins and oxidation producing the stiffening and changes to the clarity of the natural lens. In fact, cataracts have and are forming the minute you open your eyes. The triad of accommodation is miosis, esotropia, and the anterior steepening of the lens. By virtue of our inability to accommodate, in our fourth decade, we have developed cataracts. Furthermore, we have advanced the small incisions with lasers, the foldable soft acrylic intraocular lenses, the echelettes that make the lenses multifocal. However, as we noted prior with newer technology, the simplicity of selecting a multifocal lens should not be done in a vacuum. The art of choosing the best lens for our patient still relies on what is visually important and tolerant to the patient. Whereas most multifocal and trifocal lens platforms can provide good quality near and far vision, they are limited by nighttime dysphotopsia. Neural adaptation is activated to adjust to these “rings of light,” but for some that is a mountain too steep to climb. As clinicians we need to find a balance with our patients between the sequalae of glare at night, relative to a greater range of near vision without spectacles. Moreover, there are patients who have had previous corneal refractive procedures and may have macular issues or scarring that will nullify or limit the best aspects of these intraocular wonders. Thus, it is noodle time.
Fortunately, today we have even more opportunities to improve all of our patients’ quality of life. For those aforementioned cataract patients, we can now use a light delivery device to change the shape of an intraocular lens using the Light Adjustable Lens (LAL) from Rx Sight. The LAL manages the refractive error in-vivo. The LAL is a silicone, three-piece monofocal IOL that’s filled with macromers, a photosensitive material that changes the lens’ shape and power in response to ultraviolet light. This also brings the optometrist’s refracting acumen front and center in regard to the final outcome for your patient. Since they can get three bites at the apple, patients can try a modified monovision for a few weeks and decide if it is right for them, or if they had gone all distance and are unhappy with the near results, they can opt to induce some nearsightedness with LASIK-like accuracy. Furthermore, with the latest generation of this lens (LAL+) near vision may be enhanced in their distance eye. The LAL is adjustable to within 0.25D, and thus it can easily manage most patients. Patients get a refraction about two weeks after the implantation, and the LDD activates the lens prior to the final lock in. In our practice the refractions and subsequent treatments are all done by the optometrist.
Aside from the simplicity of the LAL discussion with patients, the LAL highlights the importance of optometry’s clinical contribution to the success of this new technology. The LAL may not be the only lens that provides our patients the ability to adjust the final outcome. There are other lens options in the pipeline such as the Perfect Lens, which uses low-level femtosecond laser energy to alter the hydrophilicity of a hydrophobic acrylic IOL’s polymer. It’s done in a pattern called “phase wrapping” that slowly builds a change in an IOL’s subsurface, affecting a change in the lens itself. What makes this unique is that it can make not only spherical but also toric corrections on the lens, allowing for a multifocal pattern on the lens.
Another novel idea is the ability to titrate the refractive error of materials, such as the cornea and crystalline lens. The laser-induced refractive index change (LIRIC), in its early development at the University of Rochester, in New York, uses low-level pulsed femto laser energy to non-surgically alter the refractive index of certain materials and tissues such as the cornea, crystalline lens, intraocular lenses, and contact lenses.
Fortunately, we do have better technology. However, we as a profession cannot afford to be myopic. Taking the time to read, looking at the big picture, and assessing all the information at hand is what a doctor must do. The technology is only as good as our understanding of where it fits in.