December 7, 2023
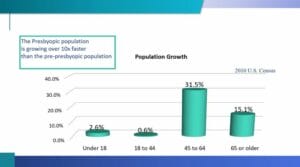
If you have read any of the articles that I have contributed to Review of Presbyopia and the Aging Eye, you will clearly know of my affinity for cataract surgery and how the procedure greatly enhances the vision and the lives of our patients. But even if you don’t have the “love “ for it like I do, you should still embrace the management of cataracts. Because, like it or not, chances are that you will see a patient with a cataract today and every day that you examine eyes. The demographic of patients who are most likely to develop a cataract is one of the fastest growing sectors in America. In 2010, 15.1% of all Americans were age 65 or older. But the results of the 2020 U.S. census indicate that this same age cohort now makes up almost 20% of the American population. It is expected that this trend will continue through at least 2050. This presents a huge opportunity for your practice, one for which you and your staff should be prepared.
Clinically, our first step in managing a patient with cataracts is to decide whether surgery is indicated for each particular patient, or if we can improve the patient’s vision adequately with an optical solution. That decision varies from patient to patient and from doctor to doctor. And it is one that should be made by the doctor and patient together. But in reality, the work of taking care of cataract patients begins way before that patient walks through your office door. Start by making sure that your entire office is ready to appropriately handle the volume of cataract patients you will be seeing. You must also be able to care for them the way they expect to be cared for these days.
Not Your Grandmother’s Cataracts
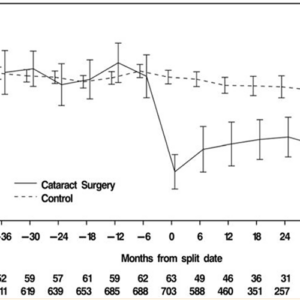
Today’s cataract patients have a different mindset and a different set of expectations than the last generation of cataract patients had. Heck, they have different goals than cataract patients from five years ago. Cataract patients are trending younger. In 2015, around 870,000 cataract extractions were performed on patients younger than 65. It is estimated that the number is now well over one million. This phenomenon is not because cataracts are developing earlier in people’s lives, rather because eye doctors are referring patients for surgery earlier in the stage of the disease because the outcomes are so good.
Visual acuity is no longer the only criteria for recommending surgery. Glare, especially when driving or when using a computer is a very common complaint of younger patients and one that can easily be addressed by removing a cataract. Night vision difficulties of any type are a common complaint of patients with early cataracts. Also, cataracts cause a demonstrable and sometimes debilitating lack of contrast sensitivity. These patients will present with decent visual acuity, (20/20- or 20/25-) but complain vociferously about poor vision and that they “just can’t see!”
When patients’ subjective complaints of their VA outweigh the objective measurements, contrast sensitivity is often the culprit. Contrast sensitivity is not a measurement that is commonly taken, but in cases like just mentioned, often a contrast sensitivity measurement will be the key to the diagnosis. Remember that VA is just a number and that many patients with “good” VA may be bothered by the subjective nuisances that cataracts can cause. As a result, what we are seeing is a trend toward earlier surgical referrals. But with these earlier referrals come loftier expectations.
The Referring Doctor’s Expanding Role
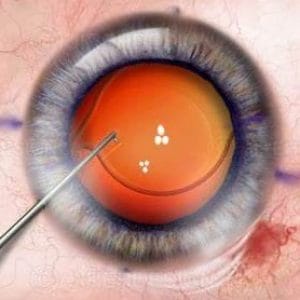
With these higher expectations come an enhanced role for the referring optometrist in the pre-operative counseling of these patients. As the primary eye care doctor, you know your patient’s eyes intimately. But you also have great insight as to the personality of the patient and what each patient expects to achieve from the cataract surgery experience. Does your patient want complete spectacle independence, or will they be perfectly happy wearing glasses for near tasks? Perhaps your patient is an avid golfer and wants exquisite vision for golfing? Or is your patient that particular person who has worn glasses their whole life and feels naked without them. These are all super important questions to which a surgeon should know the answers. But the fact is that few high-volume cataract surgeons will take the time to ask and listen to the response. This is why, again, your relationship with your patient is so important. These are questions best asked by you and shared with the surgeon prior to your patient’s consult. The decision as to which type of surgery and which IOL to have implanted should be made by you and your patient, again, prior to your patient’s appointment with the surgeon. By your taking a more active role in pre-operative counseling and in choosing the proper type of IOL for your patient, that patient is far more likely to have a positive outcome and be happier with the procedure than if you left those decisions up to the surgeon (or the surgeon’s surgical counselor).
In addition to knowing your patient, in order to do all of this effectively, you also have to know the different IOL options that the surgeon(s) to whom you refer are using. And you need to match those options to your specific patient. Realistically, those options are not decided upon solely on the basis of optical outcomes. There are emotional, intellectual, and financial aspects that need to be considered as well. Once again, you as the primary care eye doctor are in a much better situation to help your patient make this decision than anyone at the surgeon’s office, who has only seen this patient one time.
It Takes a Village
There is one more ingredient to enhancing the surgical success of your cataract patient, and that is to make your staff a part of the process. Your front office staff certainly has to know that their doctors take care of cataracts. There is far more to a successful surgical outcome than just performing the surgery. Your staff should absolutely understand and be able to communicate to a patient your role in the pre- and post-operative management of cataracts. Your technical staff also plays an integral role. They are likely the ones who will communicate all the pertinent facts to the surgeon’s office. They should be the ones to make the referral, send the requisite pre-operative notes, and fully communicate with the surgeon’s team what the patient is wanting to have done. Referring a patient with a clearly delineated game plan is far better than simply referring a patient for cataract surgery. In order to do this, your technician has to understand the different IOLs and surgeries offered. Finally, your “check out staff” needs to have a clear understanding of what is needed to bill properly for post-operative care. Suffice it to say that knowledge is essential for completing the circle of patient satisfaction.