March 20, 2024
For almost half a century, lacrimal occlusion with punctal or canalicular plugs have been used to treat dry eye disease.1 The primary indications for punctal plugs are moderate to severe aqueous deficiency dry eye and are considered a step 2 therapy according to TFOS DEWS II.
Punctal plugs are a safe and effective tool to retain the natural tear film and prolong the effect of other treatments such as artificial tears and prescription medications including cyclosporine or topical autologous serum.1 For individuals who have poor compliance or limited mobility or tremors, punctal plugs can be beneficial.

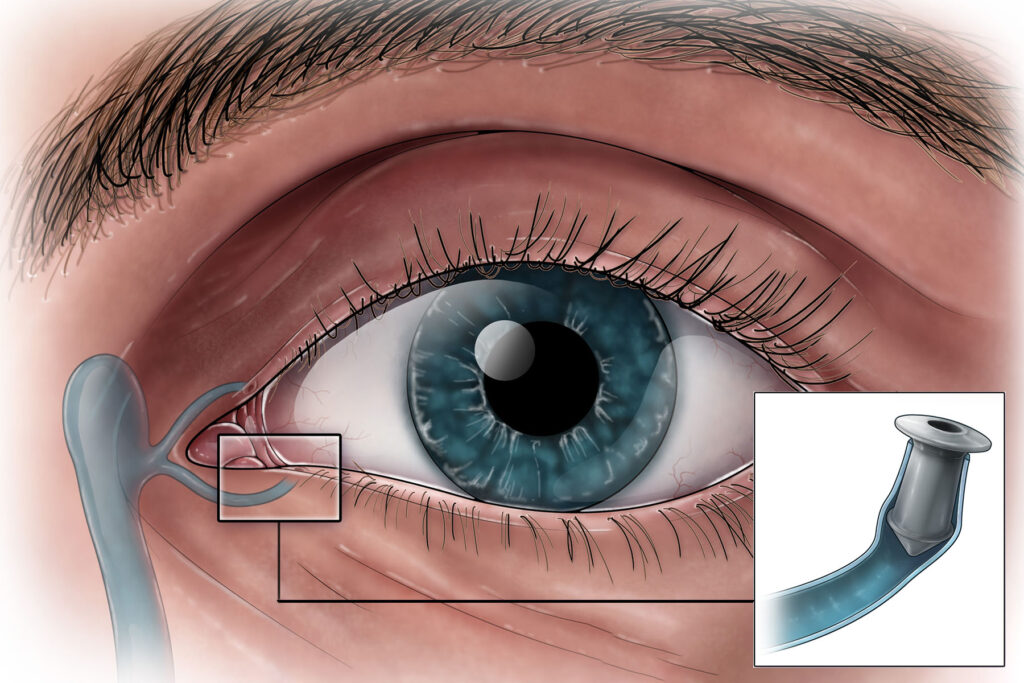
Myriad types of punctal plugs are available and differ in design, placement location (punctal versus canalicular) and resorbability. These plugs consist of collagen, silicone, hydrogels, polydioxanone, or acrylics. They are categorized into punctal and canalicular plugs based on their placement, and they are considered temporary or permanent plugs based on their longevity.
Multiple indications for punctal occlusion are dry eye disease associated with contact lens wear, superior limbic keratoconjunctivitis, or refractive surgery.2 Punctal plugs have demonstrated improvement in the management of recurrent corneal erosions and neurotrophic keratopathy.2 Additionally, plugs with perforations may be used to treat acquired punctal stenosis.
While punctal plugs are a great option for aqueous deficient dry eye patients, it is important to address any ocular surface inflammation prior to plug insertion. Trapping proinflammatory cytokines in the tear film for extended periods can potentially exacerbate ocular surface damage. However, a study involving 29 patients with moderate dry eye disease revealed that punctal occlusion for three weeks led to reduced corneal fluorescein staining and symptom scores.3 Surprisingly, the study did not find elevations of cytokine or matrix metalloproteinase-9 levels, which questions the assumption that cytokine levels inevitably rise with short-term punctal occlusion.
Novel indications for punctal plugs include extended delivery of drugs to the ocular surface. One such plug is Dextenza (dexamethasone ophthalmic insert) 0.4 mg for intracanalicular use. It is indicated for the treatment of ocular inflammation and pain following ophthalmic surgery and for the treatment of ocular itching associated with allergic conjunctivitis. Dextenza is preservative free and offers patients up to 30 days of sustained steroid coverage.
Plugs are contraindicated in patients with active ocular infection, especially keratoconjunctivitis and blepharitis, lacrimal obstruction and ectropion due to possible complications. While plugs are considered a safe therapy to treat dry eye patients, they are not without potential risks. One risk is migration of the plug into the lacrimal drainage system, which may require surgical removal of the plug.4 Infection, inflammation, epiphora, and pyogenic granulomas have all been reported with plug use.4
Although nothing we do for a patient is without risk, punctal plugs represent a valuable therapeutic option for managing dry eye syndrome, particularly for our aqueous deficient patients. Conserving the patient’s natural tears can provide relief, improve ocular surface hydration, and boost tear film. With proper patient evaluation and management, punctal plugs can significantly enhance the quality of life for individuals suffering from dry eye syndrome.
References
- Best AL, Labetoulle M, Legrand M, M’garrech M, Barreau E, Rousseau A. Punctal and canalicular plugs: Indications, efficacy and safety. J Fr Ophtalmol. 2019 Mar;42(3):e95-e104. doi: 10.1016/j.jfo.2018.12.003. Epub 2019 Jan 26. PMID: 30692031.
- Gomes JAP, Azar DT, Baudouin C, Bitton E, Chen W, Hafezi F, Hamrah P, Hogg RE, Horwath-Winter J, Kontadakis GA, Mehta JS, Messmer EM, Perez VL, Zadok D, Willcox MDP. TFOS Lifestyle: Impact of elective medications and procedures on the ocular surface. Ocul Surf. 2023 Jul;29:331-385. doi: 10.1016/j.jtos.2023.04.011. Epub 2023 Apr 20. PMID: 37087043.
- Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. Ocul Surf. 2017 Jul;15(3):575-628.
- Bourkiza, R., & Lee, V. (2012). A Review of the Complications of Lacrimal Occlusion with Punctal and Canalicular Plugs. Orbit, 31(2), 86–93. doi:10.3109/01676830.2011.648802