April 11, 2023
When we are asked how to build a dry eye clinic, the answer is easy. You already have one!
Dry eye disease is the key reason that patients see their eye care practitioners.1 The prevalence of dry eye disease can range as wide as 5% to 50%, based on the diagnostic criteria used and the population studied. However, dry eye disease is one of the most underdiagnosed and undertreated conditions in eye care.2 Thus, there is massive potential and opportunity to address this highly prevalent condition. The great news is you can start treating dry eye with little to no initial investment.
Questionnaires Provide a Baseline for Your Dry Eye Patient
Since dry eye disease can affect everyone and becomes more prevalent as we age, we evaluate every single patient for dry eye disease in our clinics. One of the easiest things to implement in your practice is the use of a dry eye questionnaire that provides valuable baseline information.
There are a variety of questionnaires such as the Standard Patient Evaluation of Eye Dryness Questionnaire (SPEED), Ocular Surface Disease Index (OSDI), Dry Eye Questionnaire (DEQ), Canadian Dry Eye Epidemiology Study (CANDEES), and the Contact Lens Dry Eye Questionnaire (CLDEQ). We recommend selecting one questionnaire that can be repeated over time. The results can alert the technician or practitioner prior to seeing the patient that extra dry eye testing may be needed during the workup, thereby streamlining workflow. (For more on dry eye questionnaires, click here: How to Use Dry Eye Questionnaires in Your Practice Review of Optometry May 15, 2022.)
Dry Eye Symptoms Are Extensive
There are myriad dry eye symptoms, including burning, stinging, itching, tearing, a sandy sensation, feelings of grittiness and/or itchiness, a foreign-body sensation, discharge, blurry or fluctuating vision, ocular injection, photophobia, eye pain and/or eye fatigue.
In addition to asking questions about standard dry eye symptoms, it is important to ask if dry mouth or arthritis symptoms exist to investigate the presence of autoimmune disease, including Sjögren’s disease, rheumatoid arthritis, and systemic lupus erythematosus. Sjögren’s disease is a chronic, autoimmune, systemic disease characterized by lymphocytic infiltration and malfunction of the exocrine glands, resulting in predominant symptoms of dry eye and dry mouth.3 Sjögren’s is a highly ubiquitous condition and is one of the most common systemic, rheumatic, autoimmune diseases, affecting up to 1.4% of adults in the United States, second only to rheumatoid arthritis in its prevalence in North America.4 Prompt diagnosis and management is pertinent due to the predominance of diffuse large B-cell lymphoma in Sjögren’s disease.5
A Thorough Slit Lamp Exam Is Open and Shut
In addition to reviewing systemic history, careful examination with particular attention to the lids, lashes, conjunctiva, and cornea is critical to determine the etiology of a patient’s dry eye complaints. Start your exam with having a patient close their eyes to rule out lagophthalmos, which will often bring morning dry eye complaints. While closed, scan the lashes for any signs of collarettes, indicating the presence of demodex, or debris/biofilm, indicating staphylococcal blepharitis. The presence of either of these create inflammation that will spread to the nearby meibomian glands.
With the patient’s eyes open, examine the lid margin for meibomian gland disease and press on the meibomian glands to see what excretes. Given that up to 86% of patients with dry eye have meibomian gland disease, it is common to see an issue in this area.6 If the meibum is not the consistency of olive oil, addressing this will improve patient symptoms.
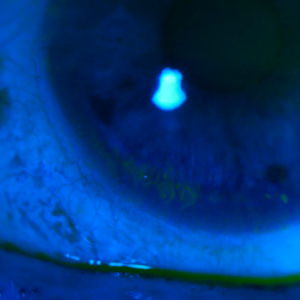
The use of vital dye testing is widely available in most clinics and can provide valuable information. With sodium fluorescein and lissamine green, look for corneal and conjunctival staining, and pull down on and evert the lids to look for lid wiper epitheliopathy as this indicates friction on the ocular surface. Assessing these structures adds very little time to your exam and will provide an excellent baseline to begin treating your dry eye patient. Starting an initial therapy and having the patient back for a more detailed dry eye workup will give you more time to better assess the ocular surface and discuss a treatment plan.
How You Treat Dry Eye Can Have a Positive or Negative Financial Impact
Ignoring dry eye in your practice can have a negative financial impact. The number of new contact lens wearers each year is roughly equal to the number of contact lens dropouts, despite improved comfort and technology with soft contact lenses.7 Studies show the most common reason patients discontinue contact lens wear is due to ocular discomfort.8 Being proactive about treating your dry eye patients builds revenue from retained contact lens patients and from any additional medical office visits and in-office treatments. As vision plans continue to decrease doctor reimbursements, moving toward a medical model can create practice growth and stability.
In-office treatments can provide incredible outcomes to treat your dry eye patients. Treatments such as microblepharoexfoliation, thermal expression, and intense pulsed light treatment can often give better results than what at-home treatments can provide. These treatments also add to your practice growth as they are often not covered by insurance and are considered cash pay procedures.
Fortunately, there is increasing awareness for both practitioners and the public of the tremendous magnitude of this condition. Treating dry eye disease can improve the quality of life for your patients and promote referrals to your practice. It is an incredible practice-building opportunity.
References
1 Gayton JL. Etiology, prevalence, and treatment of dry eye disease. Clin Ophthalmol. 2009;3:405-412.
2 Storås AM, Strümke I, Riegler MA, Grauslund J, Hammer HL, Yazidi A, Halvorsen P, Gundersen KG, Utheim TP, Jackson CJ. Artificial intelligence in dry eye disease. Ocul Surf. 2022 Jan;23:74-86. doi: 10.1016/j.jtos.2021.11.004. Epub 2021 Nov 27. PMID: 34843999.
3 Bloch K, Buchanan W, Wohl M, Bunim J. Sjogren’s syndrome: a clinical, pathological and serological study of 62 cases. Medicine (Baltimore) 1965;44:187-231.
4 Helmick C, Felson D, Lawrence R, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Arthritis Rheum 2008;58:15-25.
5 Navazesh M, Christensen C, Brightman V. Clinical criteria for the diagnosis of salivary gland hypofunction. J Dent Res 1992;71:1363-9.
6 Lemp MA, Crews LA, Bron AJ, Foulks GN & Sullivan BD (2012): Distribution of aqueous‐deficient and evaporative dry eye in a clinic‐based patient cohort: a retrospective study. Cornea 31: 472–478.
7 Andrew D. Pucker, Lisa A. Jones-Jordan, Sebastian Marx, Daniel R. Powell, Justin T. Kwan, Sruthi Srinivasan, Wolfgang Sickenberger, Lyndon Jones: Clinical factors associated with contact lens dropout. Contact Lens and Anterior Eye, Volume 42, Issue 3, 2019, Pages 318-324
8 Pucker AD, Tichenor AA. A Review of Contact Lens Dropout. Clin Optom (Auckl). 2020 Jun 25;12:85-94. doi: 10.2147/OPTO.S198637. PMID: 32612404; PMCID: PMC7323801.