July 17, 2023
With each passing year, more patients become presbyopic, with the oldest millennials (born 1981 to 1996) now crossing the 40s threshold. Millennials are now the largest adult cohort worldwide at 72.1 million, exceeding the size of the baby boomer population (ages 59 to 77) of 71.6 million.1 As these aging millennials are added to the 65.2 million people who make up Generation X (ages 42 to 57), the absolute number of presbyopes requiring vision correction will increase substantially.1,2
In 2022, the global contact lens market size was valued at 9.90 billion and is projected to grow from $10.35 billion in 2023 to $15.40 billion in 2030, a compound annual growth rate of 5.6%.3 One of the reasons for contact lens market growth is the correction of presbyopia.4 It is not shocking that presbyopia is considered an expanding revenue stream as doctors and patients alike are searching for treatment options. The demand for better presbyopia-correcting options has increased, and multifocals have continued to improve their designs to meet these needs.
The Optics of Multifocals
Multifocal contact lenses work by using different power zones across the lens surface. These optical zones have many designs, including a concentric ring design (center-near or center-distance) with multiple near zone diameters, aspheric with a progressive gradation of power throughout the lens, or extended depth of focus design. These different optical zones create the concept of “simultaneous image,” which is superimposed multiple images on the retina formed by various powers of a contact lens.5
It is well known that multifocal contact lens designs are complex, and practitioners have often had a love-hate relationship with prescribing them. Given the complexity of the optics in these lenses, it is critical that the entire eye, especially the ocular surface, is working well optically. One variable that can hinder success with multifocal contact lenses is the quality of the ocular surface.
A Good Look at the Ocular Surface
According to TFOS DEWS II, dry eye is a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles.6 The unifying feature of all dry eye disease is the disruption of tear film homeostasis, whether in the tear film, anatomy, or the nervous system.
Corneal conditions such as keratitis, epithelial basement membrane dystrophy, or scarring post refractive surgery can degrade visual quality, but the cornea isn’t the only place we should be looking. A clear cornea but poor quality tear film can also impact clarity. The tear film is a protective fluid layer on the ocular surface, containing lipids, proteins, and electrolytes.7 The lipid layer plays a vital role in the etiology and treatment of dry eye disease, and meibomian gland dysfunction alters the tear film lipid layer and contributes to tear film instability.
Changes in tear film thickness will result in an irregular air/tear interface, thus introducing aberrations into the eye’s optical system.8 Breaks in the tear film can also expose the irregular corneal epithelial surface, which may increase optical scatter.8
In addition, contact lens wear is a cause of homeostatic imbalance.9,10 A contact lens divides the tear film into the pre- and post-lens tear film. This speeds up thinning of the tear film and increases tear film evaporation.11
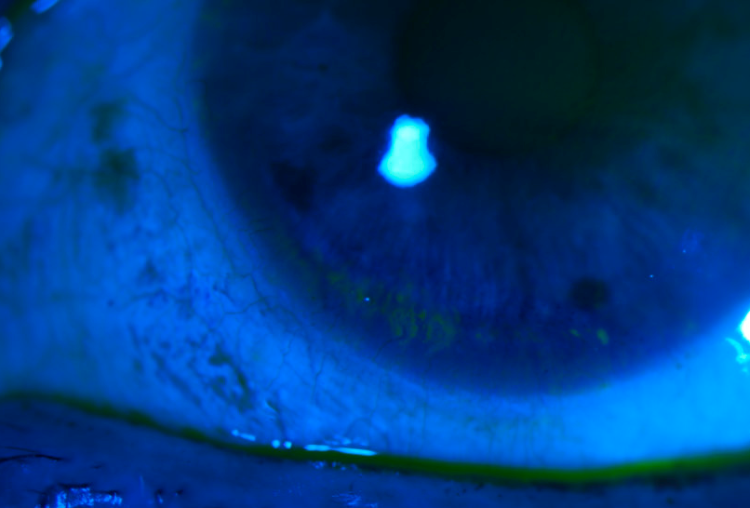
A simple test to assess the integrity of the tear film is tear break up time (TBUT). A TBUT of less than 10 seconds is abnormal and can create vision quality degradation. If available to you, noninvasive testing to evaluate the ocular surface such as corneal topography or tomography can also aid in your dry eye diagnosis. Patchy or missing areas on the reading suggest early abnormalities in TBUT. With dryness, the cornea can also become irregular, sometimes seen as inferior steepening as the corneal epithelium desicates.
The Take Home
With roughly 90% of presbyopic patients dissatisfied with their near vision,12 multifocal contact lenses can be a wonderful option to meet their needs. Addressing the ocular surface prior to multifocal fitting will save time, set better patient expectations, and improve patient outcomes. Given how common meibomian gland dysfunction, blepharitis, and demodex is in dry eye patients, a good look at the lids and meibomian glands along with the use of sodium fluorescein and lissamine green dyes will highlight any potential roadblocks in your fitting process.
References
1 Fry, Richard. Millennials overtake Baby Boomers as America’s largest generation; Pew Research Center, accessed March 2, 2023.
2 Nuefeld, Dorothy. There are 1.8 billion millennials on earth. Here’s where they live, Aging And Longevity, accessed March 2, 2023.
3 “Contact Lenses Market Size, Share & COVID-19 Impact Analysis, By Modality (Reusable, and Disposable); By Design (Toric, Multifocal, and Spherical); By Distribution Channel (Ophthalmologists, Retail Stores, and Online Stores), and Regional Forecast, 2021-20,” 2021; “Grand View Research,” 2022
4 Fricke TR, Tahhan N, Resnikoff S, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia. Ophthalmology. 2018;125(10):1-8.
5 Pérez-Prados R, Piñero DP, Pérez-Cambrodí RJ, et al. Soft multifocal simultaneous image contact lenses: a review. Clin Exp Optom. 2017 Mar;100(2):107-127. doi: 10.1111/cxo.12488. Epub 2016 Nov 1. PMID: 27800638.
6 Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II Definition and Classification Report. Ocul Surf. 2017 Jul;15(3):276-283. doi: 10.1016/j.jtos.2017.05.008. Epub 2017 Jul 20. PMID: 28736335.
7 Downie LE, Bandlitz S, Bergmanson JPG, et al. CLEAR – Anatomy and physiology of the anterior eye. Cont Lens Anterior Eye. 2021 Apr;44(2):132-156. doi: 10.1016/j.clae.2021.02.009. Epub 2021 Mar 25. PMID: 33775375.
8 Tutt R, Bradley A, Begley C, et al. Optical and visual impact of tear break-up in human eyes. Invest Ophthalmol Vis Sci. 2000 Dec;41(13):4117-23. PMID: 11095604.
9 Belmonte C, Gallar J. Cold thermoreceptors, unexpected players in tear production and ocular dryness sensations. Invest Ophthalmol Vis Sci 2011;52: 3888–92.
10 Yokoi N, Bron AJ, Georgiev GA. The Precorneal Tear Film as a Fluid Shell: The Effect of Blinking and Saccades on Tear Film Distribution and Dynamics. Ocul Surf 2014; 12:252–66.
11 Craig, JP, Willcox, MD, Argüeso, P, et al. The TFOS International Workshop on Contact Lens Discomfort: Report of the Contact Lens Interactions With the Tear Film Subcommittee. Invest. Ophthalmol. Vis. Sci. 2013;54(11):TFOS123-TFOS156.
12 Allergan survey: Allergan, an AbbVie Company, announces positive phase 3 topline results for investigational AGN-190584 for the treatment of presbyopia [press release]. AbbVie. October 28, 2020. Accessed December 15, 2020.