October 30, 2023
Over the past several years, we have seen many advances in the treatment of dry eye disease. While all these advances are wonderful for our patients, it can sometimes leave clinicians asking, which treatment do I start with? The good news is there are many correct roads to improving a patient’s symptoms as long as the first step in your treatment involves identifying the root cause of your patient’s dry eye. Discerning whether your patient has an aqueous deficiency, meibomian gland dysfunction, or a combination of both will start you on the correct path. Consider the following case.
NOMGD Case Study: ‘Non-Obvious’ MGD
A 29-year-old graduate engineering student presented for his first eye examination. He reported a history of blurry vision over the past year, both at a distance and on the computer that was worse at the end of the day. There was no history of spectacle lens wear. He reported a history of computer work for eight hours per day. He said he took occasional breaks only when he felt like they were needed. No systemic or ocular medications were taken, and there were not any known drug allergies.
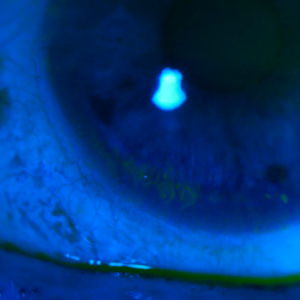
Pertinent ocular examination findings include emmetropia in each eye, 2+ meibomian gland dysfunction (MGD) with 3+ non-obvious meibomian gland dysfunction (NOMGD), and trace telangiectasia in each eye. Tear film debris was present in each eye. Tear break-up time (TBUT) was five seconds in each eye. The dilated examination was unremarkable.
With all of the dry eye treatments at our disposal, where do we start? Given this patient’s MGD and reduced TBUT, it’s clear that this patient has evaporative dry eye exacerbated by long hours on the computer.
NOMGD is a term to describe the most common form of obstructive MGD.1 Obstructive MGD is currently recognized as the most prevalent common cause of evaporative dry eye disease. NOMGD is often the precursor to evident obstructive MGD.
While there are multiple ways to target meibomian gland dysfunction (warm compresses, lid hygiene, omega-3 fatty acid supplementation, in-office thermal expression etc.), we chose to start with the new FDA-approved Miebo from Bausch + Lomb to try to stabilize the tear film.
Miebo Improved Tear Film Quality
Miebo is the first and only prescription eye drop for dry eye disease that directly targets tear evaporation. It is unique in that Miebo is a single-ingredient formulation and does not contain water. It works by forming a monolayer at the air-liquid interface of the tear film, which is expected to stabilize the natural tear film and to reduce evaporation. It can be used up to four times a day, and the eye drop size is also uniquely small, only 11 µL. According to clinical studies, Miebo improves the signs and symptoms of dry eye in as early as 15 days.
What do we expect to improve after treating our patient with Miebo? In the phase 3 clinical studies, GOBI and MOJAVE, both trials met their primary sign and symptom efficacy endpoints: change from baseline at week eight in total corneal fluorescein staining and eye dryness Visual Analog Scale score.
Success in treating dry eye hinges on two questions: 1) Did we improve the clinical findings? 2) Did we meet the patient’s goals? Improvement in meibomian gland expressibility or TBUT means nothing if the patient still has fluctuating vision or burning throughout their day. For our patient, we want to improve tear film stability, which will consequently improve blurry vision. With Miebo, the quality of the tear film improved.
We have long understood how a poorly functioning tear film is a primary contributor to ocular surface disease. MGD can initiate a cascade of inflammation, ultimately giving rise to the signs and symptoms associated with dry eyes. Having a new solution to prevent tear film evaporation can address this unmet need and keep our patients’ ocular surface healthy.
Reference
1 Blackie CA, Korb DR, Knop E, Bedi R, Knop N, Holland EJ. Nonobvious obstructive meibomian gland dysfunction. Cornea. 2010 Dec;29(12):1333-45. doi: 10.1097/ICO.0b013e3181d4f366. PMID: 20847669.
dreamstime