October 3, 2023
Many patients ask if there are modifications in their day-to-day activities that can help alleviate dry eye symptoms. While we have known for some time that lifestyle can impact the severity of ocular surface disease, the Tear Film and Ocular Surface Society (TFOS) recently published the TFOS Lifestyle report detailing the direct and indirect impact of daily lifestyle choices and challenges on ocular surface health.1 While we possess exceptional pharmaceutical treatments for assisting our patients with dry eye conditions, we consistently advocate for supplementary natural approaches to enhance a patient’s symptom relief. Minor modifications can have a significant impact, and patients might not realize that certain habits can pose challenges to the health of the surface of the eyes. Here are a few lifestyle modifications that can benefit our dry eye patients.
Physical Inactivity
While there have been conflicting findings regarding the connection between obesity and dry eye disease (DED), it’s worth noting that obesity has been linked to changes in the structure of the meibomian glands. Research has indicated that obesity is correlated with reduced tear break-up time and increased meibomian gland dysfunction, as well as higher scores on the Ocular Surface Disease Index, when compared to a non-obese control group.2
In a small human study, a 30-minute session of aerobic exercise resulted in enhancements of the Schirmer score, both invasive and non-invasive tear break-up time, and a reduction in levels of inflammation and stress markers within the tear film.3 Over a duration of 10 weeks, aerobic exercise performed three times weekly by 11 participants with dry eye disease led to an improvement in dry eye symptoms, as assessed using the 5-Item Dry Eye Questionnaire (DEQ-5).4 One proposed explanation for the beneficial effects of exercise on DED is that it may stimulate parasympathetic innervation to the lacrimal gland, particularly the acinar blood vessels, potentially increasing the secretion of electrolytes and water.5
Mask-Associated Dry Eye Disease
The term “MADE” (Mask-Associated Dry Eye) was initially coined in the early stages of the COVID-19 pandemic when numerous health care professionals began informally noting a rise in patient-reported cases of DED. A survey involving 3,605 individuals revealed that 68% of respondents experienced symptoms of mask-associated DED, with 27% of them indicating that these symptoms worsened when wearing a mask.6 Individuals wearing masks for more than six hours per day, five days per week reported a greater increase in DED symptoms (on the Ocular Surface Disease Index) from pre-pandemic scores compared to individuals who wore masks less frequently.7
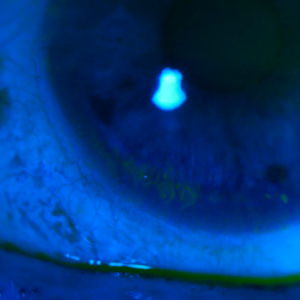
Eye Rubbing
Excessive and pathological eye rubbing can disrupt the mechanobiology of the ocular surface and the surrounding epithelium, potentially increasing the risk of developing DED. 8-9 This phenomenon, previously referred to as the “attrition concept in DED,” involves mechanical shear forces generated by rubbing, which subject the ocular surface to friction, stretching, and compression. Repeated or sustained exposure to such mechanical stresses can activate mechanoreceptors on the ocular surface, leading to sensations of pain and concurrent recruitment of neuroinflammatory mediators. Over time, the persistence of chronic inflammation due to repeated force application may contribute to the progression of dry eye disease.9
Marijuana Use
Marijuana has psychoactive properties and has found medical applications in stimulating appetite, addressing eating disorders and nausea, managing pain and chronic inflammation, as well as treating conditions such as multiple sclerosis and epilepsy.10 In humans, marijuana usage has been linked to diminished tear production11 and a reduction in corneal endothelial cell density.12 Although marijuana use may result in dry eye symptoms and decreased tear production,11 it could have potential utility in the treatment of corneal neuropathic pain.12
When managing DED in all patients, and especially those with presbyopia, keep in mind to ask about their daily activities that may impact the severity of DED.
References
1 Craig JP, Alves M, Wolffsohn JS, Downie LE, Efron N, Galor A, Gomes JAP, Jones L, Markoulli M, Stapleton F, Starr CE, Sullivan AG, Willcox MDP, Sullivan DA. TFOS lifestyle report executive summary: A lifestyle epidemic – Ocular surface disease. Ocul Surf. 2023 Aug 31:S1542-0124(23)00117-9. doi: 10.1016/j.jtos.2023.08.009. Epub ahead of print. PMID: 37659474.
2 G. Baser, N. Yildiz, M. Calan, Evaluation of meibomian gland dysfunction in polycystic ovary syndrome and obesity, Curr Eye Res, 42 (2017), pp. 661-665
3 C. Sun, X. Chen, Y. Huang, H. Zou, W. Fan, M. Yang, et al., Effects of aerobic exercise on tear secretion and tear film stability in dry eye patients, BMC Ophthalmol, 22 (2022), p. 9
4 K. Sano, M. Kawashima, S. Takechi, M. Mimura, K. Tsubota, Exercise program improved subjective dry eye symptoms for office workers, Clin Ophthalmol, 12 (2018), pp. 307-311
5 D.A. Dartt, Neural regulation of lacrimal gland secretory processes: relevance in dry eye diseases, Prog Retin Eye Res, 28 (2009), pp. 155-177
6 L. Boccardo, Self-reported symptoms of mask-associated dry eye: a survey study of 3,605 people, Contact Lens Anterior Eye (2021), Article 101408
7 S.Z. Scalinci, E. Pacella, E.T. Battagliola, Prolonged face mask use might worsen dry eye symptoms, Indian J Ophthalmol, 69 (2021), pp. 1508-1510
8 S. Masterton, M. Ahearne, Mechanobiology of the corneal epithelium, Exp Eye Res, 177 (2018), pp. 122-129
9 G.-B. van Setten, Impact of attrition, intercellular shear in dry eye disease: when cells are challenged and neurons are triggered, Int J Mol Sci, 21 (2020)
10 N.D. Volkow, R.D. Baler, W.M. Compton, S.R. Weiss, Adverse health effects of marijuana use, N Engl J Med, 370 (2014), pp. 2219-2227
11 R.S. Hepler, I.M. Frank, J.T. Ungerleider, Pupillary constriction after marijuana smoking, Am J Ophthalmol, 74 (1972), pp. 1185-1190
12 M. Mücke, T. Phillips, L. Radbruch, F. Petzke, W. Häuser, Cannabis-based medicines for chronic neuropathic pain in adults, Cochrane Database Syst Rev, 3 (2018), p. Cd012182, N. Polat, B. Cumurcu, T. Cumurcu, İ. Tuncer, Corneal endothelial changes in long-term cannabinoid users, Cutan Ocul Toxicol, 37 (2018), pp. 19-23
Getty Images