November 21, 2023
We presume that patients will inform us about their dry eye symptoms when they experience them. However, there are instances where patients may report only blurry vision as a symptom, despite having substantial keratitis. In such cases, it’s not that these patients are hiding their discomfort; rather, it could be attributed to a nerve-related issue called neurotrophic keratitis (NK).
NK is a degenerative disease characterized by corneal sensitivity reduction, spontaneous epithelium breakdown, and impaired corneal healing. It can lead to vision loss with the development of corneal ulceration, melting, and perforation.
Risk Factors Associated with NK
There are many risk factors for developing NK. Herpetic keratitis (both zoster and simplex) are the most common, but others include previous ocular surgery (i.e. LASIK, PRK, corneal transplantation, cataract surgery), chemical burns, diabetes, radiation to the eye or ocular adnexa, topical drug toxicity particularly those preserved with BAK, and contact lens abuse.1-4 While NK can be seen at any age, it is more prevalent over age 55.5,9
Why Are These Nerves Important?
Corneal homeostasis is sustained by the dynamic interplay between corneal nerves, epithelial cells and keratocytes, and the lacrimal gland.
The corneal sensory nerves release neuromediators, such as substance P, that provide trophic support to epithelial cells and keratocytes.6 Corneal sensory nerves also react to injury or insult to the ocular surface by triggering the blink reflex and the protective tear reflex by the lacrimal gland.6 Corneal epithelial cells and keratocytes release growth factors (such as NGF) and neuropeptides that influence the survival, differentiation, and maturation of nerve fibers.6 Damage to the corneal nerves can disrupt homeostasis and lead to NK.6,7
How Do We Diagnose NK?
A lack of corneal sensitivity is the hallmark clinical sign of NK. It is important to check corneal sensitivity PRIOR to the installation of anesthetic eye drops and dilation drops. However, vital dyes such as sodium fluorescein (without anesthetic) may be used prior to sensitivity testing.
While there are different methods to check corneal sensitivity, the most accurate and repeatable way to measure sensitivity is with esthesiometry. However, most clinics do not have this on hand and therefore the use of a cotton swab wisp, edge of a tissue, or even dental floss can suffice. Gently touch the cornea centrally and then in all four quadrants and compare this sensation to the other eye (if unaffected). In early stages of NK, patients may only have reduced sensitivity in one quadrant.
A thorough patient history is also beneficial to diagnose NK. Questions include a history of ocular surgery, herpetic infection, diabetes, ocular or facial surgery, chronic use of drops with BAK, and contact lens overwear. If a patient has a history of any of these conditions, it is valuable to check corneal sensitivity.
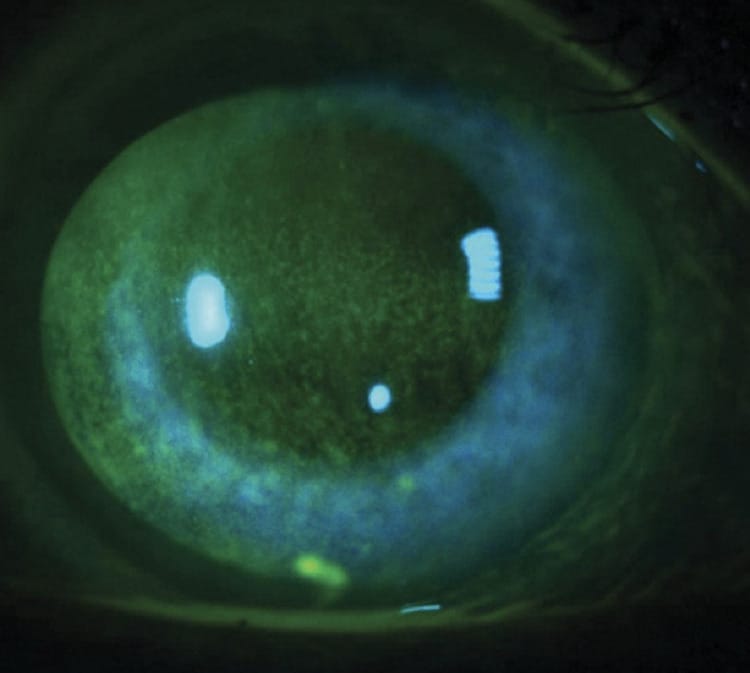
Sometimes it is challenging to differentiate dry eye disease and NK. The diagnosis is most likely dry eye if inferior corneal staining and conjunctival staining are present. If central or diffuse corneal staining is present, the diagnosis is likely to be NK.
In addition, if the clinical signs and patient symptoms don’t correlate, this raises a suspicion for NK. For example, if severe punctate epithelial keratitis or an epithelial defect is present with disproportional ocular symptoms, checking corneal sensitivity should be on your list of diagnostic testing.
Treatment of NK
Prior to 2018, the treatments for NK required surgical intervention or were palliative in nature. Thankfully, in 2018, the FDA approved cenegermin (Oxervate) as the first and only approved treatment for NK. Oxervate is a recombinant form of human nerve growth factor and is structurally identical to the nerve growth factor that is naturally produced by your eyes. Dosing is one drop six times daily in the affected eye(s) for eight weeks. In clinical trials, complete corneal healing in eight weeks was demonstrated in 70% of patients treated with cenegermin compared to 28% of patients treated without cenegermin.8
While NK is still considered a rare disease, the importance of early recognition and treatment is imperative to a positive patient outcome.
References
1 Labbe A, Alalwani H, Van Went C, Brasnu E, Georgescu D, Baudouin C. The relationship between subbasal nerve morphology and corneal sensation in ocular surface disease. Invest Ophthalmol Vis Sci 2012;53(8):4926-31.
2 Kauffmann T, Bodanowitz S, Hesse L, Kroll P. Corneal reinnervation after photorefractive keratectomy and laser in situ keratomileusis: an in vivo study with a confocal videomicroscope. German journal of ophthalmology 1996;5:508-12.
3 Wilson SE. Laser in situ keratomileusis-induced (presumed) neurotrophic epitheliopathy. Ophthalmology 2001;108:1082-7.
4 Wilson SE, Ambrosio R. Laser in situ keratomileusis-induced neurotrophic epitheliopathy. American journal of ophthalmology 2001;132:405-6.
5 Castillo-Macías A, Arreola-Martínez JE, Loya-García D, Valdez-García JE. Prevalence and clinical characteristics of neurotrophic keratopathy in hispanic population in northeastern Mexico. Int Ophthalmol. 2023 Sep;43(9):3257-3262. doi: 10.1007/s10792-023-02726-x. Epub 2023 May 4. PMID: 37140835; PMCID: PMC10400685.
6 Mastropasqua L, Massaro‐Giordano G, Nubile M, Sacchetti M. Understanding the pathogenesis of neurotrophic keratitis: the role of corneal nerves. J Cell Physiol. 2017;232:717‐724.
7 Dua HS, Said DG, Messmer EM, et al. Neurotrophic keratopathy. Prog Retin Eye Res. 2018;66:107‐131.
8 FDA approves first drug for neurotrophic keratitis, a rare eye disease. fda.gov/news-events/press-announcements/
9 Neurotrophic Keratopathy in the United States, An Intelligent Research in Sight Registry Analysis. aaojournal.org. Nov. 2022. Vol.129, No. 11