January 23, 2024
When a patient has dry eye, dry mouth, and arthritis, it is important to evaluate for autoimmune disease. This includes Sjögren’s syndrome, a persistent autoimmune systemic disease involving the entire body that is underdiagnosed in all populations, including among presbyopes. In addition to extensive ocular and oral dryness symptoms, other devastating complications resulting from this condition include profound fatigue, chronic pain, major organ involvement, neuropathies, and lymphomas.1 Although patients may present with dry eye and other symptoms, it’s possible that they may not yet be diagnosed with this condition.
Sjögren’s Syndrome Is More Common Than You Think
Sjögren’s syndrome is an extremely prevalent condition and is one of the most common autoimmune diseases, affecting up to 1.4% of U.S. adults, second only to rheumatoid arthritis (RA) in its prevalence in North America.2 There are two forms of Sjögren syndrome: primary Sjögren syndrome, when a dysfunction of the exocrine glands occurs in the absence of other autoimmune diseases; and secondary Sjögren syndrome, which is concomitant with another underlying rheumatic disease, such as systemic lupus erythematosus (SLE), RA, or scleroderma.3
In a publication by Acs, et al., it was well established that the monitoring of dry eye disease in Sjögren’s syndrome is not uniform in diverse practices.4 In a retrospective chart review from six practices in the United States and Canada, the most commonly recorded variables were dry eye symptoms (98.4% of charts), meibomian gland dysfunction (76.4% of charts), corneal fluorescein staining (75.6% of charts), and anterior blepharitis (73.2% of charts). Creating accepted standards of testing will enhance communication and understanding among practitioners and researchers to communicate and understand the course of dry eye disease in Sjögren’s syndrome.
Does Dry Eye Related to Sjögren’s Look Different from Non-Sjögren’s Dry Eye?
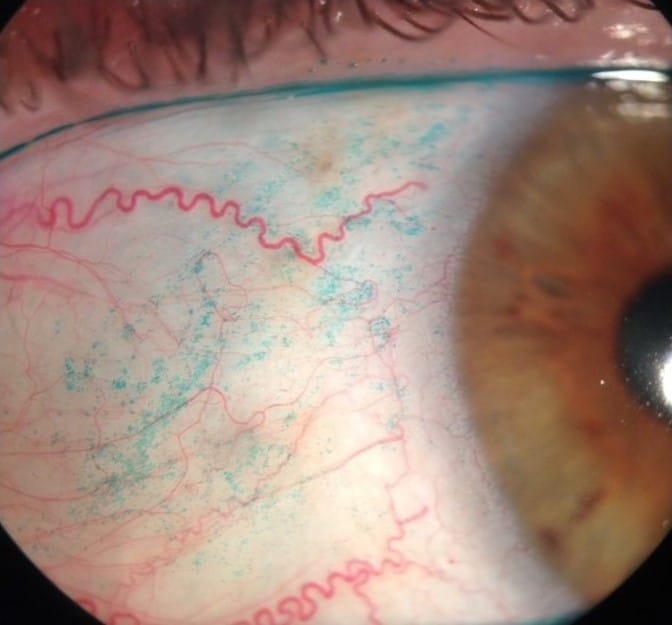
A new innovative study used anterior segment images to identify the characteristic features of Sjögren’s syndrome-related dry eye disease to create an uncomplicated method to screen for dry eye disease.5 A retrospective study of 502 eyes evaluated patients examined between August 2020 and January 2021. The study included 64 women and four men with a variety of autoimmune disorders including Sjögren’s syndrome (68), ocular graft-versus-host disease (50), other conditions (27), simple dry eye disease (72), and no dry eye disease (97).
The inferior corneal fluorescein staining score was significantly higher in the Sjögren’s syndrome group. Also, the nasal lissamine green staining score was high in the Sjögren’s syndrome group.
Thus, a high risk for Sjögren’s syndrome may be detected with positive inferior corneal fluorescein staining in combination with positive nasal lissamine green staining. Detecting these signs early may be beneficial for autoimmune-related dry eye disease, specifically Sjögren’s syndrome, and may be beneficial in the early diagnosis of Sjögren’s syndrome-related dry eye disease. Prompt diagnosis is pertinent for effective management and intervention. The limitations of this study include prominent age-related and sex-related differences in the study population and that it is a retrospective design.
Why Prompt Diagnosis is Critical
Primary Sjögren’s syndrome has been shown to affect patients’ health-related quality of life due to dryness, chronic pain, depression, anxiety, physical and mental fatigue, and neuropsychiatric symptoms.6,7
Comec et al., conducted a large, health-associated, quality of life study in a primary Sjögren’s syndrome cohort.6 Health-related quality of life impairments were severe using the 36-Item Short Form Survey. Patients with high systemic activity reported more intense symptoms. Among all symptoms, dryness, pain, and fatigue, using the European League Against Rheumatism Sjögren’s Syndrome Patient-Reported Index, demonstrated the highest scores and the strongest association with health-related quality of life.
How Do We Treat Sjögren’s Syndrome?
Myriad treatments are available to lubricate the ocular surface including over-the-counter tears, topical medications, nasal stimulation, intense pulsed light, eyelid hygiene, punctal occlusion, and autologous serum. Scleral lenses are tertiary therapy in the management algorithm but are a viable management option for patients with ocular surface disease, including Sjögren’s syndrome when other modalities are unsuccessful due to vision or comfort issues.
The Take Home
Sjögren’s syndrome is underdiagnosed in all populations, including the presbyopic population. If a patient has symptoms including dry eye, dry mouth, and arthritis, it is essential to evaluate for autoimmune disease, including Sjögren’s syndrome.
Even though there have been many advances in our knowledge of Sjögren’s syndrome, there are many potential areas of investigation.8 Various genetic and environmental risk factors as well as cellular and molecular pathways have been identified that may provide multiple targets for new systemic and ocular therapies. Technological progress has led to innovations in genetics, genomics, and epigenetic research. These novel techniques will help to recognize additional risk factors for the diagnosis, treatment, and management of Sjögren’s syndrome.
References
1 Negrini S, Emmi G, Greco M, et al. Sjögren’s syndrome: a systemic autoimmune disease. Clin Exp Med. 2022 Feb;22(1):9-25. doi: 10.1007/s10238-021-00728-6. Epub 2021 Jun 7. PMID: 34100160; PMCID: PMC8863725.
2 Helmick C, Felson D, Lawrence R, et al. Estimates of the Prevalence of Arthritis and Other Rheumatic Conditions in the United States. Arthritis Rheum 2008;58:15-25.
3 Dumusc A, Rao V, Bowman SJ. Sjögren’s Syndrome. Medicine 2018;46:126-130.
4 Acs M, Caffery B, Barnett M, et al. Customary practices in the monitoring of dry eye disease in Sjogren’s syndrome. J Optom. 2018 Oct-Dec;11(4):232-241. doi: 10.1016/j.optom.2018.05.001. Epub 2018 Jul 17. PMID: 30017867; PMCID: PMC6147754.
5 Shimizu E, Sato S, Asai K, et al. Clinical Features of Sjögren Syndrome-Related Dry Eye Disease in Anterior Segment Photographs. Cornea. 2024 Jan 1;43(1):18-25. doi: 10.1097/ICO.0000000000003342. Epub 2023 Jul 17. PMID: 37487173.
6 Cornec D, Devauchelle-Pensec V, Mariette X, et al. Severe Health-Related Quality-of-Life Impairment Inactive Primary Sjögren’s Syndrome is Driven by Patient-Reported Outcomes: Data from a Large Therapeutic Trial. Arthritis Care Res (Hoboken) 2017;69(4):528-35.
7 Lackner A, Stradner MH, Hermann J, et al. Assessing Health-Related Quality of Life in Primary Sjögren’s Syndrome-The PSS-QoL. Semin Arthritis Rheum 2018;48(1):105-10.
8 Fadel D, Barnett M. Ocular Surface Disease in Sjögren’s Syndrome: Management in a Scleral Lens Clinical Practice. JCLRS [Internet]. 2020Aug.25 [cited 2024Jan.14];4(1):e12-e22.