April 11, 2023
STAAR Surgical of Monrovia, California, has perfected its implantable intraocular lens. Yes, the ICL has been improved beyond the already existing, vision-changing, and arguably life-altering refractive status. So, all of those moderately myopic patients who you were, and are, thinking about talking with about refractive surgery options, will now have a more modernized version of the ICL. But, before we go any further, be prepared for the inevitable Baader-Meinhof phenomenon that you are going to experience . . . read on to learn more.
Whereas LASIK has made great strides with the addition of wavefront technology, the use of a femtosecond laser to create a predictable and uniform flap is still limited. Specifically, I am referring to the moderately myopic candidate, or a patient with thinner-than-comfortable corneas, tomographies, and topographies that are dubious. In these cases, corneal refractive surgery is not the best option.
If you are unaware of the phakic IOL, you are truly missing out on a refractive miracle. With correction of myopia in ranges of -3.00D to -20.00D, and astigmatism in the range of 1.00D to 4.00D, the ICL has provided contact lens and glasses relief for the forgotten patients. Furthermore, corneal-based procedures work at the fringes of the eye’s refractive borders, whereas the ICL sits as close to the nodal point as possible.
Telling Patients How the Intraocular Lens Works
My discussion to patients is simply that this lens behaves like a soft contact lens in the eye and is implanted through an incision equivalent to those made millions of times a year by cataract refractive surgeons. There is an excitement to the simplicity and elegance to the placement of this phakic lens in the ciliary sulcus. Most practitioners either don’t remember or are too young to even know that the original phakic IOLs sat in the anterior chamber. Without any removal of tissue, worry of pupil size, or possibility of any flap-related issues, coupled with the fact you could remove the lens (not sure why you would need or want to), the ICL procedure is still, almost 20 years after FDA approval, a modern improvement in refractive surgery.
I know I have painted a refractive masterpiece, however there was one drawback regarding this lens. The ICL blocked the pupil, and this extra step of creating a peripheral iridectomy (preferably preoperatively assisted with a YAG laser or the more preferred European surgical method of during the ICL implantation) was needed.
I have heard from enough patients that the YAG laser peripheral iridotomy (PI) was equivalent to being snapped by a rubber band. Now, I am sure there are a lot worse things than being snapped by a rubber band, but I am not sure that I want to volunteer to get snapped unnecessarily.
Another unfortunate side effect of the iridotomy is that they were not always large enough or full thickness that the aqueous transferred easily from the posterior to the anterior chamber, and therefore, a rise in intraocular pressure (IOP) was an unfortunate consequence. Managing these patients often meant being diligent around the implantation and the IOP. Moreover, some surgeons attempted to thwart this complication by enlarging the PIs and creating glare or, in the very rare case, some diplopia. This latter option can be the reason why some ICL patients have unwanted dysphotopsia.
The FDA-Approved Standard of Care for ICL Patients
Which brings us to the EVO ICL! As far back as 2005, when the ICL V4 was rolling out in the U.S., researchers questioned how they could avoid the PI. The addition of a 0.36 mm hole in the center of the ICL V4 optic was evaluated for both the transfer of aqueous and continuation of vision for ICL patients.
The EVO ICL has been in use outside the U.S. for over a decade, with more than a million implants worldwide. Now, the EVO is FDA approved and the standard of care for ICL patients. The availability of the EVO ICL ensures that the preoperative management of these patients is as seamless as the postoperative management. As with any refractive surgery, a thorough ocular surface evaluation is a necessity as is a discussion about expectations.
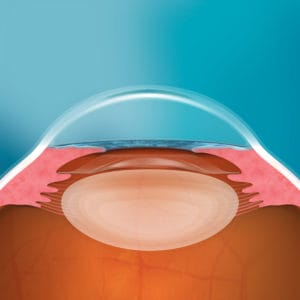
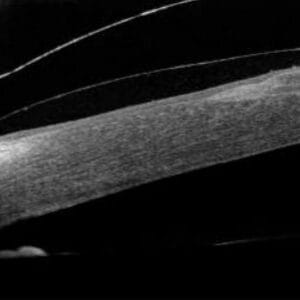
The postoperative evaluation of the lens should include visualization of the vault, the space from the posterior EVO ICL to the anterior crystalline lens, some mild anterior chamber inflammation, and IOP measurements. I traditionally see these patients at one day and one week; my one-month follow-up is often not necessary since the quality of the patient’s vision and the quiet anterior chamber make this visit unnecessary. The main emphasis on follow-ups is to make sure the toric ICL is in the correct alignment and the lens has a sufficient vault from the crystalline lens. I still use the thickness of the cornea, via purkinje images, as my “ruler” for the vault. Although it is unlikely to see the vault change, you want to know where it is as time moves forward. Without a PI, there is really very little else to evaluate except the excitement emanating from your patients’ faces.
Finally, What Is the Baader-Meinhoff Phenomenon?
STAAR plans to use the EVO platform for presbyopic ICLs and hopefully the ability to treat hyperopes in the U.S. You may have just heard this for the first time, but, as the Baader-Meinhof phenomenon predicts, something new seems to appear more frequently. Very soon you will be encountering patients you know who will benefit from the EVO ICL.