June 1, 2023
One of my favorite annual events is the Association for Research in Vision and Ophthalmology (ARVO) meeting. It is held in late April or early May, and it’s different from other conferences. It’s not a continuing education meeting, but rather it is a research conference with most attendees being academics, vision scientists, and researchers. Clinicians do attend, but they are in the minority. In addition to the invited lecturers and special interest groups, each section puts together mini symposiums, paper, and poster sessions. There are several different sections including glaucoma, retina, clinical/epidemiologic research, cornea, lens, and pharmacology, to name a few.
For three years, I was a member of the glaucoma section committee, which was responsible for putting the sections’ events together. The philosophy of ARVO is that all members should have a forum to present their research. In the fall, ARVO members submit an abstract describing their work (purpose, methods, results, conclusions). The review process occurs in December with each committee member reviewing hundreds of abstracts. Each abstract is graded by at least two committee members, with the highest scores usually going into paper sessions and the others presented as posters. The rejection rate is relatively low, as the reviewers are looking for egregious errors such as no control group, the clinical trial not being registered, the abstract being a literature review, or the results not making sense based upon study design.
The abstracts are not truly peer reviewed and, as an attendee, you learn to view certain abstracts with caution. The beauty of the meeting is that on any day, there could be a hundred posters on a topic you would like to learn more about. The attendee can read the poster, discuss it with the author(s) who remain by the poster for an advertised period, and speak with others who are reviewing it. This year’s meeting had some great glaucoma material, and I would like to discuss information I found interesting. To read about these and other abstracts, go to the ARVO website.
Comparative Outcomes of Selective Laser Trabeculoplasty
In a poster from the United Kingdom, selective laser trabeculoplasty (SLT) outcomes performed by optometrists and ophthalmologists were compared. SLT is being performed more often in the National Health Service, and records were available to assess each group’s performance. The primary outcome measure was mean intraocular pressure (IOP) reduction at 12 months. Secondary outcomes were mean change in visual acuity (VA), change in glaucoma medications, and failure outcomes. Safety outcomes were loss of two lines or more of vision or other complications. There was a statistically significant IOP reduction for both groups and no statistically significant difference in mean VA, medication use, or duration to glaucoma surgery. The relative risk of post-op SLT IOP > 21mm Hg was 3.3 times greater in the ophthalmology group. Efficacy outcomes were similar between groups, SLT delivered by optometrists was safe and effective, and an increased use of SLT by optometrists might reduce pressure on overburdened eye clinics.
Direct Selective Laser Trabeculoplasty (DLST) is a new non-invasive procedure. One poster examining IOP reduction was done by a group from Italy. Seven eyes of seven patients with primary open angle glaucoma (POAG) or ocular hypertension (OH) had DSLT performed with IOP being reduced from 28.5 mmHg to 20.6. The study’s conclusions were that DSLT reduces IOP with efficacy and safety profiles like SLT.
The GLAUrious study is a large prospective trial to assess DLST, done at 13 centers around the world. A total of 84 patients were randomized to receive DLST, and 77 received SLT. IOP reduction at six months for the DLST group was 5.46 mmHg compared with 6.16 mmHg for the SLT group. At 12 months, DSLT subjects had a mean IOP reduction of 3.20 mmHg versus 3.28 mmHg in the SLT group. No safety concerns were identified, and over half of the patients were medication free at 12 months in both groups. Conclusions were that DSLT is safe and effective and may provide an alternative to SLT. There was no reason given why efficacy reduced from six to 12 months.
Don C. Hood presented a paper examining how glaucoma progresses in the central macula. The temporal inferior sector was involved initially (significantly thinned in 82% of 62 eyes) followed by the temporal superior sector. This was followed by the middle sectors with the nasal sectors being the last involved.
Impact of Mindfulness Meditation on IOP Explored
The role of adjunctive therapies for managing open-angle glaucoma is an important topic. In a poster presented by Harvard Medical School research scholar Abdelaziz Abdelaal and colleagues, a meta-analysis of 10 randomized controlled trials was performed evaluating mindfulness meditation (MM) for lowering IOP in individuals receiving medical therapy for open-angle glaucoma (OAG). A total of 488 eyes were analyzed with the difference between MM and medically treated (MT) compared. Mean difference was 2.19 mmHg, highest at three weeks and showed a reduction over time. IOP reduction related to MM only occurred in subjects who had 30 hours or more of training, which addresses an important question of what is needed to achieve IOP reduction. High baseline IOP showed greatest reduction. Improvements were seen in cortisol, B-endorphin, and quality of life measures. While MM does not appear to lower IOP enough to be considered a primary therapy, it may provide complimentary relief for those with open-angle glaucoma.
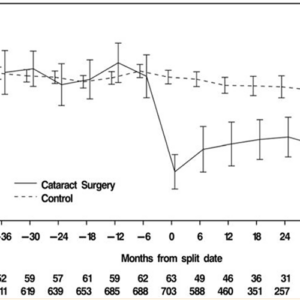
Drug delivery is an exciting area in glaucoma care. In a poster presented by individuals associated with Glaukos, the results of a single center, open-label prospective 24-month trial were presented using the Travoprost Intraocluar Implant (75 um (iDose TR). Fourteen cohorts of 15 subjects were enrolled in which an iDose TR was implanted, monitored, and exchanged with a new implant inserted at pre-determined intervals. At three months, the average amount of travoprost remaining was 60 ug (80%), six months 57 ug (75%) and at 12 months post implantation 38 ug (50%). There were no adverse events related to implant tolerability or the exchange process. The results point toward the viability of the implant being used for up to two years with excellent efficacy and safety.
There were a host of ARVO abstracts available that address home visual field testing, adherence, genetics, and new glaucoma treatments. I recommend those interested in what is new to glaucoma to review other abstracts at the ARVO website. A picture is forming of what new treatments are in development, both medical and surgical as well as the role of new diagnostic tests. ARVO is one place to see how care diagnosis and management is evolving.