October 2, 2023
According to current statistics, one in every 10 people will have Alzheimer’s dementia by the time they are 65 years old. That risk will then double every five years. Other sobering statistics from the Alzheimer’s Association reveal that one in three seniors die with Alzheimer’s or another dementia, and it kills more than breast cancer or prostate cancer combined.
At the American Academy of Optometry’s Spring 2018 meeting in San Antonio, Dr. George Perry, former dean of the College of Sciences and the Semmes Foundation Distinguished Chair in Neurobiology at The University of Texas at San Antonio, gave an intriguing lecture on Alzheimer’s disease during the Nutrition, Disease, Prevention, & Wellness Special Interest Group (SIG) Symposium. Dr. Perry is distinguished as one of the top 10 Alzheimer’s disease researchers with over 1,000 publications, and he is one of the top 100 most-cited scientists in neuroscience and behavior. He serves as editor-in-chief for the Journal of Alzheimer’s Disease, and he is the former president for the American Association of Neuropathologists.
Dr. Perry is a renegade in Alzheimer’s research. Elucidating oxidative damage as the initial cytopathological abnormality in Alzheimer’s disease, he eschews the amyloid cascade hypothesis, long considered dogma, that has driven Alzheimer’s research since 1992. The belief that deposition of amyloid β protein, the main component of the plaques in Alzheimer’s brains, is the causative agent of Alzheimer’s pathology and that the neurofibrillary tangles, cell loss, vascular damage, and dementia follow as a direct result of this deposition have led hundreds of scientists in academia and industry (at a cost of tens of billions of dollars) down the wrong path, according to Dr. Perry. His research shows that there is a relationship, but not a causal one. Plaques, he said, may be a byproduct of biological processes aimed at protecting the brain. After 30 years and $24 billion invested in efforts to reduce plaques (that have not resulted in any effective treatments for the disease), Dr. Perry’s hypothesis, considered controversial at that time, has since gained traction with recent research pointing to oxidative stress and mitochondrial dysfunction emerging as drivers of cognitive decline in all types of dementia.1,2,3,4,5,6
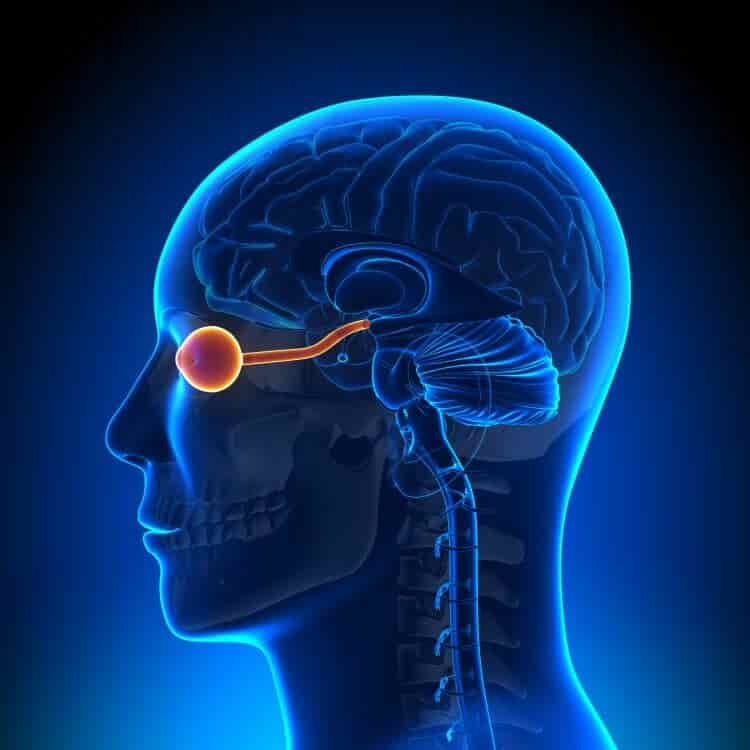
Macular degeneration is another example of a disease driven by oxidative stress and mitochondrial dysfunction. Macular drusen, which consist of lipid and calcium and build up in Bruch’s membrane, have a similar composition to the amyloid-beta plaques that form in the brains of Alzheimer’s patients. Both drusen and amyloid-beta plaques utilize the same mechanisms to damage surrounding tissue. Recent studies have pointed to a link between age-related macular degeneration, cataracts, or diabetes-related eye disease and dementia. Researchers even examined how the removal of cataracts impacted the risk for developing dementia. Emerging data strongly supports adding cataract surgery to the list of modifiable risk factors for dementia.
Recommending lifestyle interventions based on current scientific evidence is already considered standard of care for those who care for macular degeneration patients.
WHO’s Preventative Lifestyle Interventions
In July 2018, the World Health Organization (WHO) Guideline Development Group, which consisted of 21 clinicians and academic researchers from around the world, convened at the WHO headquarters in Geneva to evaluate and discuss the evidence for different dementia-prevention strategies, their potential benefits and harm, along with their costs and practicality. From this summit emerged a list of different lifestyle interventions that the WHO recommends to reduce the risk of dementia, including Alzheimer’s dementia. Their findings were published in May 2021.7
1. Physical Activity: People who are physically active have reduced risks for cognitive decline, Alzheimer’s disease, vascular dementia, and other dementias. Benefits appear greater for aerobic training compared to resistance training. For adults aged 65 years and above, the WHO recommends 150 minutes or more of moderate-intensity aerobic physical activity per week, or 75 minutes or more of vigorous-intensity aerobic physical activity per week (or an equivalent combination of both).
2. Stop Smoking: Observational studies have shown that people who smoke are at a higher risk of developing all types of dementia and up to a 79% increased risk for Alzheimer’s disease.8 Smoking is associated with higher levels of oxidative stress and mitochondrial dysfunction.8
3. Nutrition and Diet: A healthy diet is associated with larger brain volumes and better cognitive performance in aging. The WHO recommends a Mediterranean-like diet to reduce the risk of cognitive decline and dementia. A new study published in the Journal of Alzheimer’s Disease by a Virginia Tech Carilion School of Medicine faculty member shows that brain levels of dietary lutein, zeaxanthin, lycopene, and vitamin E in those with Alzheimer’s disease are half those in normal brains.9 Higher dietary levels of lutein and zeaxanthin have been strongly linked to better cognitive functions and lower risk for dementia or Alzheimer’s disease. Since the WHO met in 2018 to discuss lifestyle interventions for cognitive decline, nutrition and diet research continues to support the role of the gut-brain connection in cognitive decline. Research presented at the American Society for Nutrition 2023 in Boston showed that a certain strain of probiotics may improve cognitive function and potentially prevent age-related cognitive decline by modulating the gut microbiome.10 In this randomized clinical trial, participants with mild cognitive impairment who were given Lactobacillus rhamnosus GG probiotic over three months showed improved cognitive scores. Lactobacillus rhamnosus GG has been shown to increase beneficial bacteria and decrease pathogenic bacteria such as Prevotella, which has been shown to be elevated in cognitive impairment.11
4. Reduce Excessive Alcohol Consumption: Excessive alcohol consumption is a significant risk factor for dementia and cognitive decline.1,10 The WHO recommends interventions to stop excessive drinking such as behavioral/psychological therapies and drug treatments.
5. Cognitive Interventions: Lifelong learning is associated with cognitive health, and higher levels of cognitive activity at mid or late life are linked to delayed onset of cognitive impairment.11 The Advanced Cognitive Training for Independent and Vital Elderly, or ACTIVE, Study is the first randomized, controlled trial to demonstrate long-lasting, positive effects of brief cognitive training in older adults.12 This large trial found that community-dwelling seniors who received cognitive training had less of a decline in certain thinking skills than their peers who did not have training.
6. Social Activity: Social isolation is a risk factor not only for dementia but also for hypertension, coronary heart disease, and depression.13 Low social participation, fewer social contacts, and more loneliness have all been associated with increased dementia risk.14 Based on the current research, the WHO did not make specific recommendations for social activity to reduce the risk of cognitive decline, but they noted that social participation and social support are strongly connected to overall health and well-being.
7. Weight Management: Based on a systematic review suggesting that lifestyle interventions aimed at weight loss could improve some cognitive functions such as attention, memory, and language, the WHO made a conditional recommendation for weight management interventions in middle-aged adults but not for the elderly.1,15
8. Management of Hypertension, Diabetes, and Dyslipidemia: The WHO recommended treatment in individuals with these underlying conditions as these conditions are risk factors for cognitive decline.
9. Management of Hearing Loss: At the time of the summit in 2018, the WHO noted that there is insufficient evidence to recommend the use of hearing aids to reduce the risk of cognitive decline and/or dementia. However, a new study led by researchers at the Johns Hopkins Bloomberg School of Public Health found that older adults with greater severity of hearing loss were more likely to have dementia, and dementia was lower among hearing aid users compared to non-users.16 The findings, from a nationally representative sample of more than 2,400 older adults, are consistent with prior studies showing that hearing loss might be a contributing factor to dementia risk over time and that treating hearing loss may lower dementia risk.
Link Between Vision Loss and Dementia
Recent research has noted a link between age-related macular degeneration, cataracts, or diabetes-related eye disease and dementia. For example, one study found an increased risk of dementia in older adults who experienced worsening vision over an eight-year period.17 Another study published this year included 489,211 participants over 10 years and found that the presence of cataracts is associated with a significant increased risk of developing all-cause dementia.18 The study authors concluded that cataracts are associated with the risk of cognitive impairment and dementia, including Alzheimer’s disease and vascular dementia.19
Cataract Surgery May Prevent Dementia
A recent study published in JAMA Internal Medicine makes a strong case that removing cataracts can reduce the risk for developing dementia.20 The authors analyzed the relationship between cataract surgery and risk of dementia over time among more than 3,000 older adults with cataracts or glaucoma. None had dementia at the start of the study. The researchers found the following:
- The risk of developing dementia was 29% lower among people who had cataract surgery than among otherwise similar people who did not have the surgery.
- Among people with glaucoma, the risk of dementia was the same whether they did or didn’t have surgery.
- Study results were unlikely to be due to differences in health or access to health care, or other risks for dementia. After researchers accounted for these factors, the results were unchanged.
A 2023 prospective cohort study of 300,823 participants over 8.4 years published in Biological Psychiatry showed a 50% reduction in all-cause dementia risk in those who received cataract surgery vs. those who did not. Additionally, cataract was negatively associated with cortical volumes, aging-related subcortical volumes, and fractional anisotropy of white matter fibers.21
While more research is still needed, strong data supports the link between vision loss and cognitive decline. The available data strongly suggests that removal of cataracts can protect patients from cognitive decline.
Health Span vs. Life Span
Life span is the number of years someone lives from birth until death, while health span is the number of years someone is healthy without chronic and debilitating disease. Lengthening health span starts with being proactive in following guidelines that are evidence-based ways to promote health and vitality vs. reactive and waiting until symptoms begin. Addressing vision issues early with cataract removal can increase health span. The percentage of Americans over 65 years old continues to increase, and it is more important now than ever that practitioners be armed with recommendations to increase not only life span but health span, too. Eye doctors are therefore on the front lines of aging well.
References
1 Mizrani A, Tabassum S, Yang L. Mitochondrial dysfunction and oxidative stress in Alzheimer’s disease. Front. Aging Neurosci., 18 February 2021. Volume 13.
2 Cassidy L, Fernandez F, Johnson J et al. Oxidative stress in Alzheimer’s disease: a review on emergent natural polyphenol therapeutics. Complementary Therapies in Medicine. Volume 49, March 2020
3 Mao P. Oxidative stress and its clinical applications in dementia. Journal of Neurodegenerative Diseases, Volume 2013, Article ID 319898.
4 Ionescu-Tucker A, Cotman C. Emerging roles of oxidative stress in brain aging and Alzheimer’s disease. Neurobiology of Aging, Volume 107, Nov 2021, 86-95.
5 Rebecca Power, John M. Nolan, et al. Omega-3 fatty acid, carotenoid and vitamin E supplementation improves working memory in older adults: A randomised clinical trial. Clinical Nutrition. 2021 Dec.; volume 41, issue 2, 405-414,
6 Rebecca Power, John M. Nolan, et al. Targeted Nutritional Intervention for Patients with Mild Cognitive Impairment: The Cognitive impAiRmEnt Study (CARES) Trial 1. Journal of Personalized Medicine. 2020 May 25
7 WHO (2019) WHO Guidelines: Risk reduction of cognitive decline and dementia.
8 Anstey KJ, von Sanden C, Salim A et al. (2007) Smoking as a risk factor for dementia and cognitive decline: a meta-analysis of prospective studies. AM J Epidemiol 166, 367-378.
9 Dorey CK, Gierhart D, Fitch KA et al. Low xanthophylls, retinol, lycopene, and tocopherols in grey and white matter of brains with Alzheimer’s disease. J Alzheimers Dis. 2023;94(1):1-17.
10 Aljumaah MR, Bhatia U, Roach J et al. The gut microbiome, mild cognitive impairment, and probiotics: A randomized clinical trial in middle-aged and older adults. Clin Nutr. 2022 Nov;41(11):2565-2576.
11 Langballe EM, Ask H, Holmen J et al. (2015) Alcohol consumption and risk of dementia up to 27 years later in a large, population-based sample: the HUNT study, Norway, Eur J Epidemiol 30, 1049-1056.
12 Vemuri P, Lesnick TG, Przybelski SA et al. (2014) Association of lifetime intellectual enrichment with cognitive decline in the older population. JAMA Neurol 71, 1017-1024.
13 Willis SL et al. (2006) Long-term effects of cognitive training on everyday functional outcomes in older adults: The ACTIVE Study. Journal of the American Medical Association, 296:2805-2814.
14 Livingston G, Sommerlad A, Ortega V et al. (2017) Dementia prevention, intervention, and care. Lancet.
15 Kuiper JS, Zuidersma M, Oude Voshaar RC, et al. (2015) Social relationships and risk of dementia: A systematic review and meta-analysis of longitudinal cohort studies. Ageing Res Rev 22, 39-57.
16 Veronese N, Facchini S, Stubbs B et al. (2017) Weight loss is associated with improvements in cognitive function among overweight and obese people: A systematic review and meta-analysis. Neurosci Biobehav Rev 72, 87-94.
17 Huang AR, Jiang K, Lin F, et al. Hearing loss and dementia prevalence in older adults in the US. JAMA. 2023;329(2):171-173.
18 Shang X, Zhu Z, Huang Y, et al. Associations of ophthalmic and systemic conditions with incident dementia in the UK Biobank. Br J Ophthalmol 2021 Sep13.
19 Luping W, Bowen S, Zheng Z. (2023) The risk of dementia or cognitive impairment in patients with cataracts: a systematic review and meta-analysis. Aging and Mental Health, DOI: 10.1080/13607863.2023.2226616.
20 Lee CS, Gibbons LE, Lee AY, et al. Association between cataract extraction and development of dementia. JAMA Intern Med 2022 Feb 1;182(2):134-141.
21 Ma Ling-ZHI, Zhang Ya-Ru, Li Yu-Zhu, et al. Cataract, cataract surgery, and risk of incident dementia: a prospective cohort study of 300,823 participants. Biological Psychiatry. 2023;93(9):810-819.
Medscape