October 25, 2023
The American Nutrition Association’s 2023 annual meeting convened in Charlotte, N.C. this month. The theme was Personalized Nutrition: Healthy Aging & Longevity. Cardiologist Dr. Dariush Mozaffarian, MD, DrPH, dean emeritus of Tufts University’s Friedman School of Nutrition Science and Policy and director of the newly launched Food is Medicine Institute at Tufts, gave an intriguing lecture describing recent research findings about the correlation and impact of poor-quality nutrition on chronic disease management and prevention, particularly for diabetes and cardiovascular disease. Recent studies have also shown that a poor diet has a significant impact on ocular health, and as practitioners who routinely care for aging eyes, it’s important for us to be well versed in basic patterns of eating and nutrition that promote health and well-being. Dr. Mozaffarian shared the following eye-opening statistics:
Diet-Related Disease in the U.S.
More U.S. Adults are Sick Than Are Healthy
- 1 in 2 have diabetes or prediabetes
- 3 in 4 are overweight or obese
- Only 1 in 15 (6.8%) are metabolically healthy
Sick American Teenagers:
- 1 in 4 have prediabetes
- 1 in 4 are overweight or obese
- 1 in 6 have fatty liver disease
A Failing Grade on Nutrition:
- Average Healthy Eating Index (HEI) score: 58 out of 100
- No age, sex, racial, ethnic, or income subgroup has an HEI score > 65
- Diet quality worst at ages 5-18 years
Poor Nutrition, a Horrific Impact:
- Kills 10,000 Americans each week
- Causes 21,000 new cases of diabetes each week
- Causes 45% of all cardiometabolic deaths
(U.S. Burden of Disease Collaborators, JAMA 2018; O’Hearn et al., JACC 2022; O’Hearn et al., Nature Med 2023; Centers for Medicare & Medicaid Services, 2018; American Heart Association, Heart Disease and Stroke Statistics, 2018; The Milken Institute, America’s Obesity Crisis, 2018)
After a decade on the faculty at Harvard, Dr. Mozaffarian was recruited to Tufts in 2014 to serve as the Dean of Tufts Friedman School of Nutrition Science and Policy, where he helped propel evidence-based research in nutrition. He is one of the top cited researchers in medicine globally, and in 2023, Dr. Mozaffarian was nominated by President Biden to serve on the President’s Council on Sports, Fitness, and Nutrition (PCSFN), a federal advisory committee that aims to promote healthy eating and physical activity for all Americans. Dr. Mozaffarian’s lecture on Food is Medicine at the American Nutrition Association’s conference was a wake-up call for practitioners and policy makers. He referenced the Global Burden of Disease (GBD) study that was published in The Lancet in 2019, which showed that our food is the number one cause of death globally.1 Dietary patterns listed in the study that were most contributory to disease are as follows:
- Diets high in sodium
- Diets low in whole grains
- Diets low in fruits
- Diets low in nuts and seeds
- Diets low in vegetables
- Diets low in seafood omega-3 fatty acids
- Diets low in fiber
- Diets low in polyunsaturated fatty acids
- Diets low in legumes
- Diets high in trans fatty acids
- Diets low in calcium
- Diets high in sugar-sweetened beverages
- Diets high in processed meats
- Diets low in milk
- Diets high in red meat
Dr. Mozaffarian also referenced a recently published study in Nature Medicine 2023, where the authors show that the global burden of type 2 diabetes is attributable to suboptimal intake of 11 dietary factors as follows: insufficient intake of whole grains, excess intake of refined grains, excess intake of processed meats, excess intake of unprocessed red meat, insufficient intake of yogurt, excess intake of sugar-sweetened beverages, excess intake of potatoes, insufficient intake of fruit, insufficient intake of nuts and seeds, insufficient intake of non-starchy vegetables, and excess intake of fruit juice.2
Per the Tufts Food is Medicine Institute, poor diets are the leading cause of death in the U.S. with Americans with lower incomes, living in rural communities, and from historically marginalized racial and ethnic groups most affected. Poor diets are also harming our economy. The combined health care spending and lost productivity from suboptimal diets cost the economy $1.1 trillion each year with roughly 85% of all health care spending related to the management of diet-related chronic diseases. Each year, the direct medical costs of diabetes are $237 billion, and another $90 billion is lost from reduced productivity. These figures exceed the annual budgets of many federal departments and agencies, including, among others, the USDA, NIH, CDC, and FDA combined. Yet, studies show that type 2 diabetes is largely treatable and preventable with good nutrition.
Eye Doctors on the Front Lines of Patient Education and Prevention
Thanks to the National Institues of Health/National Eye Institute AREDS and AREDS2 trials, we as a profession have long understood the impact that proper nutrition can have on the course of disease. Spanning over 20 years and changing the standard of care for practitioners who care for patients with AMD, these trials showed that certain nutrients can slow the progression of intermediate to advanced AMD, the number one cause of vision loss in the developed world. The 10-year post hoc analysis of the AREDS and AREDS2 patients showed the importance of overall dietary eating patterns such as the Mediterranean diet with fatty fish twice a week for preserving retinal function.
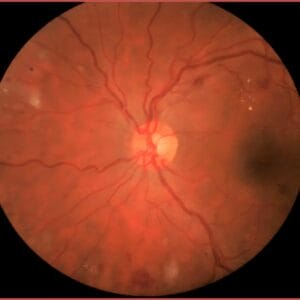
William Shakespeare said that the eyes are the window to your soul, but they are so much more than that. Eyes are the windows to the vascular system. Problems spotted in the retina are often the first signs of disease lurking elsewhere in the body. For example, population-based analyses have demonstrated the predictive value of retinal microvascular indices, as measured through photography, in screening for heart attack and stroke.3 Retinal imaging such as color fundus photography takes a few minutes per patient and allows practitioners to view the health of the vascular system up close without a lot of tissue overlying it. As the only human tissue allowing a direct, noninvasive in vivo visualization of the microvascular circulation and central nervous system, the neurosensory retina affords a unique setting for the characterization of systemic disease.3 Microvascular changes precede clinical manifestation and are independent predictors for hypertension, diabetes, coronary disease, renal disease, and stroke.3,4,5,6,7 These retinal images can then be used as teaching tools for patients to show the importance of lifestyle practices that influence vascular health such as nutrition and exercise.
My article, “Early Cognitive Decline: Can Eye Doctors Mitigate the Risk Through Lifestyle and Vision Interventions?,” discussed mitigating cognitive decline in aging through lifestyle interventions. Retinal imaging has given practitioners the ability to identify those at risk of early cognitive decline early at a time when lifestyle changes may still have a chance to mitigate the course of disease. Alterations in the thickness of the retinal nerve fiber layer and macular volume, most easily revealed through optical coherence tomography (OCT), may highlight those individuals most at risk of developing cognitive decline and neurodegenerative disease.8,9,10,11 Research in lifestyle interventions such as exercise and diet are proving to be powerful interventions in promoting not just life span but also health span.
Follow the Nutrition Science
Nutrition science is exploding, and we now have evidence-based nutrition recommendations that have been shown to preserve the health of the vascular system, which affects every retinal disease seen clinically. For example, per Pubmed/Medline, from 2001-2010 there were approximately 13,000 newly published scientific papers on diet and cardiovascular disease, whereas close to 27,000 were newly published between 2011-2020. For diet and obesity, around 15,000 scientific papers were published from 2001-2010, whereas approximately 48,000 papers were newly published from 2011-2020. Pubmed/Medline data also show that published studies on diet and diabetes from 2010-2020 more than doubled from the previous 10-year period. The retinal imaging technology afforded to eye care practitioners that can be done quickly on every patient provides one of the most valuable teaching tools for vascular health in medicine.3 We as a profession can no longer afford not to embrace the opportunity we have to not only change the course of disease but also to reduce the burden of health care costs by embracing prevention.
References
1 Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019). Seattle, United States: Institute for Health Metrics and Evaluation (IHME), 2020.
2 O’Hearn M, Lara-Castor L, Cudhea F et al. Global Dietary Database. Incident type 2 diabetes attributable to suboptimal diet in 184 countries. Nat Med. 2023 Apr;29(4):982-995. PMID: 37069363.
3 Wagner SK, Fu DJ, Liu X et al. Insights into systemic disease through retinal imaging -based oculomics. Transl Vis Sci Technol. 2020 Feb 12;9(2):6.
4 Wong TY, Mohamed Q, Klein R et al. Do retinopathy signs in non-diabetic individuals predict the subsequent risk of diabetes? Br J Ophthalmol. 2006; 90:301-303.
5 Gunthner R, Hanssen H, Hauser C et al. Impaired retinal vessel dilation predicts mortality in end-stage renal disease. Circ Res.(Published online April 1, 2019)
6 McGeechan K, Liew G, Macaskill P et al. Meta-analysis: Retinal vessel caliber and risk for coronary heart disease. Ann Intern Med. 2009; 152: 404-413.
7 Wong TY, Mitchell P. Hypertensive retinopathy. N Engl J Med. 2004; 351: 2310-2317.
8 Thomson KL, Yeo JM, Waddell B et al. A systematic review and meta-analysis of retinal nerve fiber layer change in dementia, using optical coherence tomography. Alzheimer’s Dement (Amst). 2015; 1: 136-143.
9 Mutlu U, Colijn JM, Ikram MA et al. Association of retinal neurodegeneration on optical coherence tomography with dementia: a population-based study. JAMA Neurol. 2018; 75: 1256-1263.
10 Ko F, Muthy ZA, Gallacher J et al. Association of retinal nerve fiber layer thinning with current and future cognitive decline: a study using optical coherence tomography. JAMA Neurol. 2018; 75: 1198-1205.
11 Coppola G, Renzo A, Ziccardi L et al. Optical coherence tomography in Alzheimer’s disease: a meta-analysis. PLoS One. 2015; 10: e0134750.
Dreamstime