August 8, 2023
“There comes a point where we need to stop just pulling people out of the river. We need to go upstream and find out why they’re falling in.” -Bishop Desmond Tutu
In 1900, life expectancy hovered around 50 years of age with most people dying from “fast” causes such as accidents, injuries, and infectious diseases. Since then, slow death has supplanted fast death with most people in developed countries dying from chronic diseases such as heart disease, cancer, neurodegenerative disease, or type 2 diabetes and metabolic dysfunction. In fact, per CDC data from the National Center for Health Statistics, heart disease and cancer alone are responsible for 46% of deaths in the United States. Almost half of the U.S. population, or 133 million Americans, are living with at least one chronic condition, and over 40% are living with two or more with the numbers continuing to grow.1
Our current medical model does a very good job at treating acute injuries and illness and has even developed prevention strategies that save lives from “fast causes.” It’s the law to wear our seat belts while riding in cars because research has shown that it saves lives. We wear our helmets while skiing down black diamond runs going anywhere from 25-50 mph, and just as diligently we wear our helmets while leisurely biking on a Sunday afternoon. We have mighty weapons in antiseptics and antibiotics that have proven effective against acute illnesses. Indeed, we have gotten great at avoiding death from “fast” causes. While it is apparent in the medical literature that modifiable lifestyle practices now account for roughly 80% of premature mortality, our current medical model does a poor job at preventing death from the slow causes of chronic diseases. Why aren’t we more focused on preventing the onset of disease?
Post-Traumatic Growth
Looking back in history, a phenomenon of positive transformation often occurs after a society has experienced a collective trauma. The Black Death pandemic (1347-1350) that devastated Europe shook Italian society and transformed it. People moved out of the big cities such as Florence. The sense that life was fleeting and that every happiness should be seized led many Italians to seek solace in art and literature, and thus the Renaissance was born. Life was transformed. Post-traumatic growth is the theory that explains this kind of transformation. It was developed by psychologists Richard Tedeschi, Ph.D. and Lawrence Calhoun, Ph.D. in the mid-1990s, and it holds that people or societies who endure psychological struggle following adversity can often see positive growth afterward.
On May 11, 2023, the U.S Department of Health and Human Services declared an official end to the COVID-19 public health emergency that has plagued humanity since 2020. What is emerging from the collective trauma of the COVID-19 pandemic is a thirst for knowledge on ways to strengthen health and prevent disease. In an opinion piece for Newsweek, Harvard professor Dr. Beth Frates urged the public to look to lifestyle medicine for extra protection from COVID’s worst effects. Patients and practitioners alike now have a deeper appreciation for health and wellness. COVID-19 woke society up to the fact that having a chronic illness such as diabetes or heart disease increases vulnerability and hastens mortality. This awareness has sparked another Renaissance, a Renaissance of health.
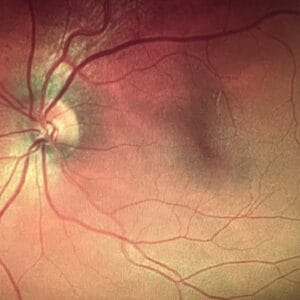
Diet and Supplements Can Prevent AMD
It is important that practitioners understand not just the treatment of disease but also ways to help patients prevent them from happening in the first place. Science is now showing us evidence-based ways to work “upstream” at preventing morbidity and mortality from the chronic diseases that are plaguing society and driving up health care costs. The Mediterranean diet is one of the most extensively studied patterns of eating, and it has been shown to lower inflammation and be protective against many diseases such as cardiovascular disease and macular degeneration.
The National Institutes of Health/National Eye Institute’s Age-Related Eye Disease Studies (AREDS and AREDS2) focused on preventing the progression of macular degeneration with the results showing that the AREDS formula of nutrients showed a clinically significant reduced risk of progression from intermediate to advanced AMD. Their randomized controlled trials changed the standard of care for the most common cause of vision loss in the developed world. In 2021, a 10-year post hoc analysis of the AREDS and AREDS2 was published.2 The main aim of this post hoc analysis was to use the AREDS data to examine potential associations between the dietary intake of multiple nutrients and progression to late AMD, including a separate analysis of geographic atrophy and neovascular AMD. The results strengthened the previous evidence for protective associations between dietary intake of specific nutrients and the risk of late AMD. Their findings showed a decreased risk of AMD progression with the following nutrients: vitamins A, D, E, C; B vitamins such as folate, B6, B12, thiamine, riboflavin, niacin; carotenoids, minerals such as magnesium, calcium, zinc, iron, and copper; and fatty acids from fish or algae sources. The following nutrients showed an increased risk of AMD progression: cholesterol, saturated fats, omega 6s, vegetable seed oils, and arachidonic acid. The post hoc analysis, as compared to the original studies, examined overall eating patterns and showed that a Mediterranean diet has the following benefits for AMD patients:
1. Eating a Mediterranean diet, particularly at least two servings per week of fatty fish, may be beneficial for those with early or even intermediate AMD.
2. A diet high in fish can reduce the chances of developing late AMD by 65% for patients who also have protective genes.
3. In the general AMD population, a high fish diet reduced progression of intermediate AMD, with bilateral large drusen, to geographic atrophy by 31%.
4. High adherence to a Mediterranean diet reduced progression from intermediate to late AMD, with geographic atrophy or neovascularization, by 25 to 40%.
The striking difference between the original AREDS and AREDS2 trials and the recently published 10-year post hoc analysis is the progression of geographic atrophy. The original trials did not show a benefit for geographic atrophy, but the post hoc analysis of eating patterns showed that certain patterns of eating can significantly reduce the risk of progression of geographic atrophy, and these associations are stronger for GA than neovascular AMD. Upstream interventions such as those evidenced in the PREDIMED and AREDS/AREDS2 post hoc analysis have the power to transform patient’s lives. It has been reported in studies that of all the senses, most people are more fearful of losing their eyesight than any of the other senses. Practitioners of the future will be more focused on upstream care or prevention of disease.
“My doctor told me to stop having intimate dinners for four…unless there are three other people.” -Orson Welles
| Upstream Care, the Power of Personalized Nutrition In his address announcing the new collaboration between the Ocular Wellness & Nutrition Society and the American Nutrition Association (ANA), The New York Times bestselling author, Dr. David Perlmutter, MD, FACN, ABIHM, discussed the power of nutrition in promoting wellness and preventing disease, especially as it relates to ocular health. Nutritional biochemistry has shown us that there is not a one-size-fits-all approach to diet. The American Nutrition Association is offering advanced training in personalized nutrition for practitioners. The Personalized Nutrition Practitioner Training Program and Certification is a concise, clinically focused educational program to arm practitioners with the skills and knowledge to apply personalized nutrition in practice. Ocular Wellness & Nutrition Society members receive a 35% discount on the cost of the Personalized Nutrition Training Program and Certification through the ANA. |
“Repair the Roof Before it Starts Raining” -Dr. Stuart Richer
References
1 Raghupathi W, Ragupathi V. An Empirical Study of Chronic Diseases in the United States: A Visual Analytics Approach to Public Health. Int J Environ Res Public Health. 2018 Mar 1;15(3):431.
2 Agron E, Mares J, Clemons T, et al. Dietary Nutrient Intake and Progression to Late Age-Related Macular Degeneration in the Age-Related Eye Disease Studies 1 and 2. Ophthalmology. 2021 Mar;128(3):425-442.
Getty Images