March 4, 2024
Hippocrates (c. 460 BC – c. 370 BC) is regarded as the father of modern medicine. Although he lived around 2,400 years ago, his aphorisms are still widely used today. A new frontier of medicine, microbiome research, is supporting Hippocrates’ claim that all disease (including ocular disease) begins in the gut. Recent studies support the existence of a gut-retina axis involved in the pathogenesis of several chronic progressive ocular diseases, including age-related macular disorders, showing that the health of the eyes is linked to the health of the intestines.
Gut Microbiome at a Glance
- The human gastrointestinal tract is one of the largest interfaces between the host, antigens, and environmental factors in the human body.
- The gastrointestinal microbiome represents a complex micro-ecosystem of bacteria, protozoa, fungi, algae and multicellular parasites that is integrated into a macro-ecosystem of the host with whom it interacts in a symbiotic way.
- The gut microbiome contains one hundred trillion viable microorganisms, which is 10 times the number of cells in the human body.
- While the human genome consists of approximately 23,000 genes, the gut microbiome encodes more than three million genes and produces thousands of metabolites.
- Weighing 1-1.5 kg, the gut microbiome can be considered an additional human organ rivaling the liver for the number of biochemical reactions in which it participates.
- The most important component of the gastrointestinal microflora is believed to be the colonic microflora where 95% of our microbiome is located. From the duodenum to the rectum, an increasing quantitative microbial gradient and a decreasing qualitative microbial gradient occur, also showing a progressive reduction of aerobic bacteria in favor of obligate anaerobes.1,2
- The gut microbiome comprises a few phyla such as Firmicutes, Bacteriodetes, Actinobacteria, Proteobacteria, Fusobacteria, and Verrucomicrobia, with the two phyla Firmicutes and Bacteroidetes representing more than 80-90% of the entire gut microbiome.1
- The gut microbiome drives immune function by “educating” the immune system to be both tolerant to self and reactive to pathogens.3 It shifts T-helper cell balance towards Th-1, resulting in decreased production of IgE and eosinophils, dampened hypersensitivity reactions and intestinal inflammation, greater oral tolerance, and prevention of atopic disease. It also stimulates non-specific immune stimulation by increasing production of cytokines, tumor necrosis factor alpha, and interleukin 6. It also increases production of macrophages and stimulates phagocytosis.
- The gut microbiome produces short-chain fatty acids (SCFAs) through the fermentation of unabsorbed carbohydrates in the colon. These SCFAs such as butyrate have many systemic health benefits such as anti-inflammatory, immunoregulatory, anti-obesity, anti-diabetes, anti-cancer, cardiovascular protective, hepatoprotective, and neuroprotective activities.4
- Colonic microflora produce substantially more polyamines (putrescine, spermidine, and spermine) than endogenous sources. Polyamines facilitate cell growth and differentiation; regulate RNA, DNA, and protein synthesis; and can be used as an instant energy source by intestinal cells.
- The gut microbiome is involved in digestion and nutrient absorption and produces vitamins in the B and K groups.
- The gut microbiome facilitates xenobiotic metabolism aiding in absorption and proper functioning of phytoestrogens, lignans, flavonoids, and some medicinal herbs.
- The diversity of our diets dictates the diversity of our microbiomes. A more diverse microbiome is associated with less chronic inflammation and better health overall.
- A dysfunctional gut is one of the biggest drivers of chronic, systemic inflammation. Gut dysbiosis leads to increased gut permeability, elevated circulation of bacterial products, microbial metabolites, and inflammatory mediators that result in immune dysregulation at distance anatomic sites, including the retina.
The Gut-Retina Axis
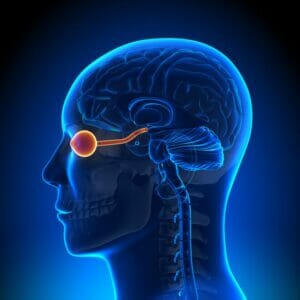
The presence of a gut microbiome-brain-retinal axis refers to a bidirectional communication network between gut and brain (and retina) strongly mediated by the immune system.1 This network is not only anatomical, but it extends to include endocrine, humoral, metabolic, and immune routes of communication. Its composition includes gut microbiota and their metabolic products, enteric nervous system, sympathetic and parasympathetic branches, neural-immune system, neuroendocrine system, and central nervous system.
The eye, specifically the retina, is an extension of the brain. The mechanisms behind gut microbiome changes and ocular diseases can be explained by several mechanisms, including the following: dysbiosis-induced increased intestinal permeability, allowing microbes and their metabolites to reach the ocular system, inducing ocular cell inflammation; dysbiosis-induced breakdown of the blood-retinal barrier responsible for increased oxidative stress in the retina; and inflammatory processes associated with age-related gut dysbiosis contributing to premature senescence of retinal cells, which, through releasing pro-inflammatory cytokines and angiogenic factors, leads to neo-vascularization and disruption of vascular repair.6,7,8
Age-related changes to the gut microbiome drive “inflammaging,” the low-grade inflammation linked to the aging process. The microbiota of long-lived elderly people and centenarians differs from frail elderly people. Long-lived people have more diversity and a decrease in proinflammatory bacteria. The aging microbiome is typified by the following changes: reduced microbial diversity; increased number of potentially harmful pathogenic bacteria; and a reduction in the production of anti-inflammatory, health-promoting SCFA metabolites such as butyrate as the numbers of beneficial bacteria that produce them decreases.9
CHANGES IN GUT FLORA→ DYSBIOSIS→ GUT INFLAMMATION→ GUT DYSFUNCTION (INTESTINAL PERMEABILITY) → SYSTEMIC INFLAMMATION→ NEUROINFLAMMATION→ DISPARATE PATHOPHYSIOLOGICAL ALTERATIONS
Aberrations in the gut microbiota (dysbiosis) and its metabolites induce systemic inflammation via stimulation of both the innate and adaptive response of the immune system. Evidence obtained from human and animal studies provides a unifying paradigm of a vicious cycle:5
Age-Related Macular Degeneration
Studies of gut dysbiosis have revealed significant changes in bacterial composition and diversity between states of health and macular degeneration.10 There is growing evidence that environmental factors associated with AMD progression potentially work through the intestinal microbiota.11 Studies on the use of probiotics to modulate retinal health are showing promising results. For example, Lactobacillus paracasei KW3110 is a strain of lactobacillus that has been particularly studied for its eye benefit. This strain has been shown to suppress retinal inflammation by reducing cytokine-producing macrophages and the loss of age-related retinal cells.1,12 Likewise, other experiments demonstrated the ability of the Lactobacillus paracasei to suppress inflammation on photoreceptor cells in a murine model of light-induced retinopathy.12 More research on human subjects needs to be done before a specific probiotic is recommended for macular degeneration patients, but emerging data suggests that the future management of macular degeneration may very well involve prescribing strain-specific bacteria to support retinal health.
Other retinal disorders that have been shown to be linked to gut dysbiosis include the following: diabetic retinopathy, retinopathy of prematurity, central retinal artery occlusion, and retinal dystrophies.13
It’s the Sum of the Parts: The Mediterranean Diet as a Prescription for a Healthy Microbiome
The naturalist John Muir, who co-founded the Sierra Club, was quoted as saying, “When we try to pick out anything by itself, we find it hitched to everything else in the universe.” This saying is applicable to all life on both a “macro” and “micro” level. The association between gut health and ocular disease is complex, involving multiple facets of microbial communities’ interactions with host cells and tissues. Metagenomics, metatransriptomics, metaproteonomics, and metametabolomics are key methodologies now being used to uncover these relationships, each providing unique insights into the complexities of microbial communities’ composition, function, and impact on host health. These more holistic approaches reveal the importance of microbial diversity in maintaining ocular health.
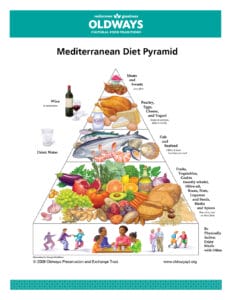
Diet has a major impact on gut microbiota, with estimates of almost 60% of the total structure of gut microbiota at least amenable to rapid modification in response to dietary changes, in as little as 72 hours.14,15,16 High animal protein diets, high fat diets, and diets high in refined carbohydrates have been shown to contribute to dysbiosis. On the other hand, the Mediterranean diet, which is high in green vegetables and fish and lower in simple carbohydrates, plays a role in shifting gut microbial composition, favoring greater diversity and higher levels of beneficial SCFAs, thereby reducing systemic inflammation and inflammaging. Mediterranean diets have been shown to be protective in AMD and other chronic diseases of aging. A heavily plant-based diet such as the Mediterranean diet high in vegetables, fruit, and fiber is key to supporting a diverse, healthy inner ecosystem. Many if not most beneficial microorganisms are plant eaters. We need a rainbow of plant foods each day, and the more species we consume, the better for our microbial diversity.
We also need to increase fiber. The average American consumes only around 15 grams of dietary fiber a day, which is well below the 25 to 38 grams recommended by the USDA’s Dietary Guidelines for Americans. Our ancient ancestors consumed between 100 to 150 grams of fiber per day. Dr. Eric Alm of MIT found that adding just 10 more grams of dietary fiber per day led to 11% more diversity in our microbiota.
In summary, studies have shown that a Mediterranean diet increases microbiome diversity, which equates to an increase in SCFAs, an increase in gut homeostasis, a decrease in gut dysbiosis, a decrease in opportunistic pathobionts, and a decrease in intestinal permeability. These changes decrease systemic oxidative stress, inflammation, metabolic syndrome, obesity, Type 2 diabetes, cardiovascular disease, macular degeneration, diabetic retinopathy, neurodegenerative disorders, and colorectal cancers with concomitant increases in insulin sensitivity and immune function.14,16,17
“Let Food be thy Medicine and Medicine be thy Food” — Hippocrates
References
1 Scuderi G, Troiani E, Minnella A. Gut microbiome in retina health: the crucial role of the gut-retina axis. Front. Microbiol. (2022) 12:726792.
2 Clarke G, Sandhu KV, Griffen BT, et al. Gut reactions: breaking down xenobiotic-microbiome interactions. (2019) Pharmacol. Rev. 71, 198-224.
3 Thaiss CA, Zmora N, Levy M, and Elinav E. The microbiome and innate immunity. (2016) Nature 535, 65-74.
4 Xiong RG, Zhou DD, Wu SX, et al. Health benefits and side effects of short-chain fatty acids. Foods. 2022 Sep15;11(18):2863.
5 Daulatzai MA. Non-celiac gluten sensitivity triggers gut dysbiosis, neuroinflammation, gut-brain axis dysfunction, and vulnerability for dementia. CNS & Neurological Disorders-Drug Targets, 2015, 14, 110-131.
6 Napolitano P, Filippelli M, Davinelli S et al. Influence of gut microbiota on eye diseases: an overview. Ann Med. 2021 Dec;53(1):750-761.
7 Wastyk H, Fragiadakis GK, Perelman D, Sonnenburg ED et al. Gut-microbiota-targeted diets modulate immune status. Cell. 2021;184, 4137-4153.
8 Wilmanski T, Rappaport N, Earls JC et al. Blood metabolome predicts gut microbiome alpha-diversity in humans. Nat. Biotechnol. 2019;37,1217-1228.
9 O’Toole PW, Jeffrey LB. 2015. Gut microbiota and aging. Science 350. 1214-1215.
10 Zhang Y, Wang T, Zhongqi W et al. Alterations of the intestinal microbiota in age-related macular degeneration. (2023) Front. Microbiol. 14:1069325.
11 Lin P, McClintic SM, Nadeem U et al. Review of the intestinal microbiota in age-related macular degeneration. J Clin Med. 2021 May 12;10(10):2072.
12 Morita Y, Miwa Y, Sakamoto A, et al. (2018). Long-term intake of Lactobacillus paracasei KW3110 prevents age-related chronic inflammation and retinal cell loss in physiologically aged mice. Aging 10, 2723-2740.
13 Xiao J, Zhang J, Amin S et al. The gut microbiome’s impact on the retina. Review of Ophthalmology. 10 May 2022.
14 Merra G, Noce A, Marrone G et al. Influence of Mediterranean diet on human gut microbiota. Nutrients 2020,13, 7.
15 Zhang C, Zhang M, Wang S et al. Interactions between gut microbiota, host genetics, and diet relevant to development of metabolic syndromes in mice. ISME J. 2010, 4, 232-241.
16 Barber TM, Kabisch S, Pfeiffer A et al. The effects of the Mediterranean diet on health and gut microbiota. Nutrients 2023, 15, 2150.
17 Nagpal R, Shively CA, Register TC, Craft S, Yadav H. Gut microbiome-Mediterranean diet interactions in improving host health. F1000Res. 2019 May 21;8:699. doi: 10.12688/f1000research.18992.1. PMID: 32704349; PMCID: PMC7359750.