March 19, 2024
Vitamin D deficiency is one of the most common nutrient deficiencies, affecting an estimated 41.6% of the total United States population.1 Minorities fare much worse, with an estimated 82.1% of Blacks and 69.2% of Hispanics affected.1 Additionally, older adults are at a much greater risk of being deficient.2 Overall, vitamin D deficiency is a silent epidemic. The symptoms are usually subtle and may take years or decades to surface.
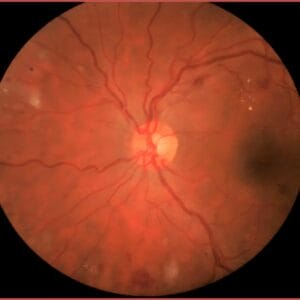
In the United States, studies have shown that vitamin D deficiency is a driver of both systemic and ocular inflammation. Vitamin D acts as an antioxidant, an immunomodulator, a regulator of angiogenesis and apoptosis, and directly or indirectly regulates up to 5% of the human genome or over 900 different genes.3 It is well established that oxidative stress, inflammation, and angiogenesis play a critical role in the development and progression of macular degeneration and other disorders of the aging retina such as diabetic retinopathy. Vitamin D deficiency plays a key role in all of these.
In a 2019 paper by Tohari et al., “Vitamin D Attenuates Oxidative Damage and Inflammation in Retinal Pigment Epithelial Cells,” the researchers examined the ability of vitamin D to protect RPE cells from oxidative stress and reduce inflammation. Cells were challenged with a strong oxidant, H2O2, and treated with vitamin D (versus control cells). Vitamin D was shown to suppress oxidative damage and inflammation in RPE cells. It significantly increased cell viability through antioxidant signaling pathways.4
Optimal vitamin D levels have been shown to reduce the risk and severity of diabetic retinopathy. In a 2021 review paper by Valle et al., vitamin D’s role in diabetic retinopathy was explored. The paper, “Protective role of vitamin D against oxidative stress in diabetic retinopathy,” looked at the molecular mechanisms by which vitamin D protects the eye from oxidative stress. The authors point out that in the last few decades, it has been reported that vitamin D is involved in the pathogenesis of diabetic retinopathy. The authors cite data showing that vitamin D modulates the production of advanced glycosylated end products (AGEs), as well as several pathways, including protein kinase C, the polygon pathway leading to the reduction of free radical formation. It also prevents the translocation of nuclear factor kappa B, preventing the inflammatory response, acting as an immunomodulator, and modulating autophagy and apoptosis.5
In a recently published systematic review that looked at vitamin D and ocular disease, the authors searched two databases for articles examining the relationship between vitamin D deficiency and different ocular diseases. Out of the 162 studies found, evidence on the association between vitamin D and myopia, macular degeneration (AMD), diabetic retinopathy, and dry eye syndrome were found.6
Overall, 17 out of 27 studies reported an association between vitamin D and AMD, while 48 out of 54 studies reported that vitamin D was associated with diabetic retinopathy. An association between vitamin D and dry eye syndrome was found in 25 out of 27 studies.
The authors noted that vitamin D regulatory enzymes are present in ocular tissues, and studies have demonstrated that ocular tissues can activate and regulate vitamin D. Their findings highlight the importance of vitamin D in maintaining ocular health, however, more research is needed.
Vitamin D and Diabetes
The Centers for Disease Control and Prevention National Diabetes Statistics Report 2023 estimates that between one in two and one in three American adults have prediabetes while diabetes affects 11.6% of the U.S. adult population. Vitamin D’s role in diabetes has been extensively studied. Vitamin D sufficiency is essential for insulin release, insulin sensitivity, reduction of inflammation, and reduction of arterial stiffness.7-12 Deficiency reduces insulin sensitivity and increases the risk of atherosclerosis, cardiovascular disease, type 2 diabetes mellitus, and hypertension.13-17 Vitamin D plays an important role in pancreatic β-cell function.13,14 By stimulating pancreatic beta cells, 1,25–dihydroxy vitamin D triggers the secretion of insulin.11,12 Clinical trials show improvements in insulin sensitivity and HbA1c when patients were given vitamin D3.17 Vitamin D supplementation has been shown to decrease C-reactive protein (CRP) and high-sensitive-CRP.18 Despite strong data supporting the importance of vitamin D sufficiency in diabetes, clinical trials of vitamin D supplementation in diabetes have been mixed. The National Institutes of Health Vitamin D Fact Sheet for Health Professionals states that clinical trials have shown little evidence to date that vitamin D supplementation improves health outcomes in diabetes in vitamin D replete individuals.
Vitamin D Characteristics
Vitamin D is a fat-soluble vitamin that functions as a pro-hormone. It enhances the intestinal absorption of calcium and phosphorus, promotes bone mineralization and remodeling, and is involved in regulating serum calcium and phosphorus levels. Vitamin D also plays a role in neuromuscular function and immune function, and it influences cellular growth and differentiation. Adequate vitamin D levels reduce systemic inflammation, while systemic inflammation reduces vitamin D absorption. In addition, vitamin D enhances the secretion and action of insulin, making it important in blood sugar control.19
There are two types of vitamin D. Vitamin D3 (also known as cholecalciferol) is synthesized in the skin from 7-dehydrocholesterol after exposure to sunlight or other sources of ultraviolet light. Vitamin D2 (also called ergocalciferol) is produced by irradiation of ergosterol, a sterol present in fungi. While vitamin D2 is not normally present in the human body and is found only in trace amounts in plants, it has vitamin D activity and has been used for decades to prevent and treat vitamin D deficiency in humans. Both vitamins D2 and D3 raise serum levels of vitamin D as measured as 25(OH)D, and they seem to have equivalent ability to cure rickets. In addition, most steps in the metabolism and actions of vitamins D2 and D3 are identical. However, most evidence indicates that vitamin D3 increases serum 25(OH)D levels to a greater extent and maintains these higher levels longer than vitamin D2, even though both forms are well absorbed in the gut.20-24
Throughout most of human history, vitamin D was obtained almost exclusively from cutaneous biosynthesis since typical diets contained little or no vitamin D. People who are exposed to adequate amounts of sunlight typically do not require a dietary source of vitamin D, however, increasing time spent indoors has contributed to global vitamin D deficiency.
Food Sources of Vitamin D
Few foods are naturally rich in vitamin D3. The best sources are the flesh of fatty fish and fish liver oils. Smaller amounts are found in egg yolks, cheese, and beef liver. Certain mushrooms contain some vitamin D2. Many foods and supplements are fortified with vitamin D, such as dairy products and cereals. The following foods are rich sources of vitamin D:
- cod liver oil
- salmon
- swordfish
- tuna fish
- orange juice fortified with vitamin D
- dairy and plant milks fortified with vitamin D
- sardines
- beef liver
- egg yolk
- fortified cereals
Testing Vitamin D Levels
Serum concentration of 25(OH)D is currently the main indicator of vitamin D status. Serum 25(OH)D is expressed in two different units: ng/ml and nmol/L. There is some controversy though over whether serum 25(OH)D is a reliable indicator of vitamin D status. In his book Nutritional Medicine, nutrition expert Dr. Alan Gaby, MD, argues that serum 25(OH)D levels decline (sometimes by 40% or more) in response to inflammation, and in people who have one of the many health conditions associated with acute or chronic inflammation, serum 25(OH)D may not be a reliable indicator of vitamin D status.19 He also argues that substantial variations in 25(OH)D results have been encountered in nearly identical samples from one laboratory to another and with the use of different methods of assessment (in-house radioimmunoassay vs. commercially available radioimmunoassay). He argues that while very low and very high 25(OH)D levels may be reasonably reliable indicators of vitamin D deficiency and excess, respectively, basing clinical decisions on serum 25(OH)D levels between those extremes may not be appropriate.
Supplementing Vitamin D
The optimal dose of vitamin D remains a topic of considerable debate. Studies have shown that 800 IU/day is more effective than 400 IU/day with respect to preventing falls and fractures in the elderly.19 Many factors need to be taken into consideration such as age, skin color (darker skin absorbs less vitamin D), amount of sunlight exposure, and other factors. In his book Nutritional Medicine, Dr. Gaby states that supplementing with 800-1,200 IU/day of supplemental vitamin D is usually safe without measuring 25(OH)D levels. However, many patients need higher doses depending on other factors.
Since vitamin D is fat soluble, it may accumulate in tissues and produce toxic effects after supplementation with large doses. Manifestations of vitamin D toxicity may include hypercalcemia, hypercalciuria, fatigue, anorexia, nausea, vomiting, polyuria, polydipsia, and cardiac arrhythmias. Calcification of the kidneys may develop and may progress to renal failure.19 Most published cases of frank vitamin D toxicity with hypercalcemia have involved an intake of 25,000 to 40,000 IU/day.19 Serum and urinary calcium levels should be monitored in patients receiving high doses of vitamin D.
As eye doctors on the frontlines of caring for patient’s most precious sense, their sight, we must be knowledgeable of current research in nutrition. The Ocular Wellness & Nutrition Society has partnered with the American Nutrition Association to provide doctors with a path to become certified in personalized nutrition through their CPNP program. Targeted evidence-based supplementation of necessary nutrients has been shown to mitigate the course of ocular disease, but it must be prescribed based on each individual patient’s needs.
- Forrest KY, Stuhldreher WL. Prevalence and correlates of vitamin D deficiency in US adults. Nutr Res. 2011 Jan;31(1):48-54. PMID: 21310306.
- Linnebur SA, Vondracek SF, Vande Griend JP, et al. Prevalence of vitamin D insufficiency in elderly ambulatory outpatients in Denver, Colorado. Am J Geriatr Pharmocother. 2007 Mar;5(1):1-8. PMID: 17608242.
- Wang, T-T, Tavera-Mendoza LE, Laperriere D, et al. Large-scale in silico and microarray-based identification of direct 1,25-hydroxyvitamin D3 target genes. Mol. Endocrinol. 2005;19:2685-2695.
- Tohari, A. M., Alhasani, R. H., Biswas, L., Patnaik, S. R., Reilly, J., Zeng, Z., & Shu, X. (2019). Vitamin D Attenuates Oxidative Damage and Inflammation in Retinal Pigment Epithelial Cells. Antioxidants (Basel, Switzerland), 8(9), 341.
- Valle MS, Russo C, Malaguarnera. (2021). Protective role of vitamin D against oxidative stress in diabetic retinopathy. Diabetes/Metabolism Research and Reviews/Volume 37, Issue 8.
- Hei-Nga Chan, Xiu-Juan Zhang, Xiang-Tian Ling et al. Vitamin D and ocular diseases: a systematic review. International Journal of Molecular Science. 2022, 23, 4226.
- Perez-Lopez FR. Vitamin D: the secosteroid hormone and human reproduction. Gynecol Endocrinol. 2007;23(1):13–24.
- Carvalho JTG, Schneider M, Cuppari L, et al. Cholecalciferol decreases inflammation and improves vitamin D regulatory enzymes in lymphocytes in the uremic environment: A randomized controlled pilot trial. PLoS One. 2017;12(6):e0179540.
- Dong Y, Stallmann-Jorgensen IS, Pollock NK, et al. A 16-week randomized clinical trial of 2000 international units daily vitamin D3 supplementation in black youth: 25-hydroxyvitamin D, adiposity, and arterial stiffness. J Clin Endocrinol Metab. 2010;95(10):4584–4591.
- Witham MD, Dove FJ, Dryburgh M, et al. The effect of different doses of vitamin D(3) on markers of vascular health in patients with type 2 diabetes: a randomised controlled trial. Diabetologia. 2010;53(10):2112–2119.
- Sergeev IN, Rhoten WB. 1,25-Dihydroxyvitamin D3 evokes oscillations of intracellular calcium in a pancreatic beta-cell line. Endocrinology. 1995;136(7):2852–2861.
- Kramer CK, Swaminathan B, Hanley AJ, et al. Prospective associations of vitamin D status with beta-cell function, insulin sensitivity, and glycemia: the impact of parathyroid hormone status. Diabetes. 2014;63:3868–3879.
- Rashidi B, Hoseini Z, Sahebkar A, Mirzaei H. Anti-Atherosclerotic Effects of Vitamins D and E in Suppression of Atherogenesis. J Cell Physiol. 2017;232(11):2968–2976.
- Chiu KC, Chu A, Go VL, Saad MF. Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction. Am J Clin Nutr. 2004;79(5):820–825.
- Bonakdaran S, Rokni H. Diabetic CVD–focus on vitamin D. Cardiovasc Hematol Agents Med Chem. 2012;10(3):241–250.
- Boucher BJ. Vitamin D insufficiency and diabetes risks. Curr Drug Targets. 2011;12(1):61–87.
- Li X, Liu Y, Zheng Y, Wang P, Zhang Y. The effect of vitamin D supplementation on glycemic control in type 2 diabetes patients: a systematic review and meta-analysis. Nutrients. 2018;10(3):375.
- Yu Y, Tian L, Xiao Y, Huang G, Zhang M. Effect of vitamin D supplementation on some inflammatory biomarkers in type 2 diabetes mellitus subjects: a systematic review and meta-analysis of randomized controlled trials. Ann Nutr Metab. 2018;73(1):62–73.
- Gaby AR. (2017). Nutritional Medicine, Second Edition. Fritz Perlberg Publishing. 113-123.
- Tripkovic L, Lambert H, Hart K, Smith CP, Bucca G, Penson S, et al. Comparison of vitamin D2 and vitamin D3 supplementation in raising serum 25-hydroxyvitamin D status: A systematic review and meta-analysis. Am J Clin Nutr 2012;95:1357-64. [PubMed abstract]
- Lehmann U, Hirche F, Stangl GI, Hinz K, Westphal S, Dierkes J. Bioavailability of vitamin D2 and D3 in healthy volunteers, a randomised placebo-controlled trial. J Clin Endocrin Metab 2013;98:4339-45. [PubMed abstract]
- Logan VF, Gray AR, Peddie MC, Harper MJ, Houghton LA. Long-term vitamin D3 supplementation is more effective than vitamin D2 in maintaining serum 25-hydroxyvitamin D status over the winter months. Br J Nutr 2013;109:1082-8. [PubMed abstract]
- Tripkovic L, Wilson LR, Hart K, Johnsen S, de Lusignan S, Smith CP, et al. Daily supplementation with 15 µg vitamin D2 compared with vitamin D3 to increase wintertime 25-hydroxyvitamin D status in healthy South Asian and white European women: A 12-wk randomized, placebo-controlled food-fortification trial. Am J Clin Nutr 2017;106:481-90.
- National Institutes of Health Office of Dietary Supplements. Vitamin D Fact Sheet for Health Professionals.