July 3, 2023
Intense pulsed light (IPL) therapy has been the standard treatment for rosacea, flushing, and facial redness, as well as manifestations of photodamage, including pigmented lesions,1 in dermatology for decades. IPL therapy is utilized by eye care professionals to treat aging changes due to photodamage, ocular rosacea, and most recently meibomian gland dysfunction (MGD) in dry eye disease. In the Tear Film and Ocular Surface Society, TFOS DEWS II treatment algorithm, the management and therapy subcommittee placed IPL as a step two treatment for dry eye and MGD.2
MGD is a chronic diffuse disease, commonly characterized by terminal duct obstruction with qualitative or quantitative changes in the glandular secretion. It can result in alteration of the tear film, symptoms of eye irritation, clinically apparent inflammation, and ocular surface disease.3 Increased tear evaporation, tear hyperosmolarity, increased ocular surface staining, increased inflammation, symptomatic irritation of the eyelid and globes, as well as decreased visual acuity have all been observed with MGD.4
MGD is often accompanied by ocular rosacea. One study reported that 80% of facial rosacea patients suffer from MGD, and in 20% of patients, ocular rosacea precedes facial rosacea.5 IPL therapy is very effective in managing rosacea and is thought to minimize the blood vessels that are responsible for leaking inflammatory mediators onto the ocular surface.6
 Figure 1: Telangiectasia and subsequent ocular rosacea
Figure 1: Telangiectasia and subsequent ocular rosacea
There are thought to be many factors that contribute to MGD. Inflammation, microbial/demodex infestation, enzyme changes, stasis, hyperkeratinization, temperature changes, and obstruction are thought to contribute whether individually or in conjunction with one another.7 IPL is still being studied on how it specifically improves MGD, but there are many retrospective and prospective studies in the literature that support the improvement in both signs and symptoms of MGD. IPL is step one in my clinic where I choose to incorporate interventional dry eye strategies. I decrease inflammation with IPL and then perform intelligent heat with expression utilizing the TearCare system.
Hordeola and chalazia can also be treated effectively with IPL. In my clinic experience, the longer the chronicity of the lesion the more treatments will be required to diminish the chalazia. Patients are usually very keen on this approach as it is less invasive than a needle (steroid injection) or a blade (incision and cutterege).
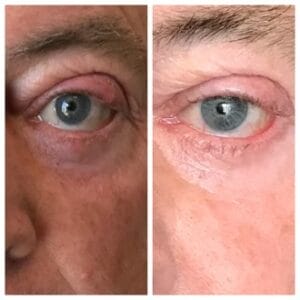 Figure 2: Before and after IPL series for chronic chalazia
Figure 2: Before and after IPL series for chronic chalazia
How does IPL mechanistically work in treating rosacea and MGD-associated dry eye? Potential mechanisms of IPL that can achieve clinical improvement include selective photothermolysis of abnormal blood vessels below the skin surrounding the eyes, activation of fibroblasts, and enhancing the synthesis of new collagen fibers. It also helps by decreasing surface demodex and the bacterial load on the eyelids, interference with the inflammatory cycle by regulation of anti-inflammatory agents and matrix metalloproteinases, reducing the turnover of skin epithelial cells, and decreasing the risk of physical obstruction of the meibomian glands. Patients not only enjoy the benefit of treating their MGD but also enjoy the benefit of improved skin texture, reduced redness, and less evidence of photodamaged skin.
 |
 |
Figure 3A and Figure 3B: Immediate before and after images show a reduction in telangiectasias in the malar region
Due to having a multifactorial etiology, dry eye disease (DED) historically has been challenging to treat. Challenge equals opportunity for eye care providers now that we have technology and medications that allows us to have a targeted approach. Many patients will have ocular rosacea, demodex blepharitis, meibomian gland dysfunction, AND dry eye disease. These can all be treated with targeted therapy for each etiology. Due to its multifactorial nature, it is possible that multiple treatment mechanisms of action are helping to reduce patient signs and symptoms of MGD and DED. As IPL expands and is utilized more to treat MGD and DED, the eye care community will continue to embrace this technology. I personally have greatly enjoyed giving my patients every opportunity to see and look their very best!
References
1 Bitter PH. Noninvasive rejuvenation of photodamaged skin using serial, full-face intense pulsed light treatments. Dermatol Surg. 2000;26:835–842.
2 Nelson JD, Craig JP, Akpek EK, et al. TFOS DEWS II introduction. Ocul Surf. 2017;15(3):269-275.
3 Kelly K. Nichols, Gary N. Foulks, Anthony J. Bron, Ben J. Glasgow, Murat Dogru, Kazuo Tsubota, Michael A. Lemp, David A. Sullivan; The International Workshop on Meibomian Gland Dysfunction: Executive Summary. Invest. Ophthalmol. Vis. Sci. 2011;52(4):1922-1929.
4 Chhadva P, Goldhardt R, Galor A. Meibomian Gland Disease: The Role of Gland Dysfunction in Dry Eye Disease. Ophthalmology. 2017;124(11S):S20-S26. doi:10.1016/j.ophtha.2017.05.031
5 Schaller M, et al. Rosacea treatment update: recommendations from the global ROSacea COnsensus (ROSCO) panel. BJD 2016 Nov 12. 465-471.
6 Papageorgiou P, Clayton W, Norwood S, Chopra S, Rustin M. Treatment of rosacea with intense pulsed light: significant improvement and long-lasting results. Br J Dermatol. 2008;159(3):628–632.
7 Geerling G, Baudouin C, Aragona P, et al. Emerging strategies for the diagnosis and treatment of meibomian gland dysfunction: Proceedings of the OCEAN group meeting. Ocul Surf. 2017;15(2):179-192. doi:10.1016/j.jtos.2017.01.006