May 30, 2023
Aging is a natural process that affects every individual, and the delicate skin around the eyes, or the periocular region, is one of the first areas to show signs of aging. Fine lines, wrinkles, and crow’s feet can make our patients feel self-conscious and detract from their overall appearance. In a trained injector’s hands, results with neurotoxin can be quite satisfying, but utilization of the medication in certain muscles can cause or exacerbate dry eye disease. This is one reason why optometrists should fight to include this procedure in their scope of practice. Optometrists, with our extensive knowledge of the anatomy and function of the periocular region, are well-positioned to administer neurotoxin injections with the utmost precision.
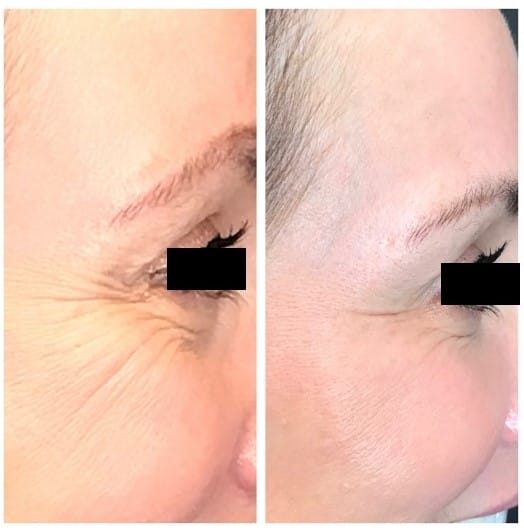
Neurotoxins are derived from the bacterium Clostridium botulinum. Serotype A is the type most widely commercially available.1 This substance works by temporarily preventing muscle contractions through blocking the release of acetylcholine leading to a relaxation of the muscles. Relaxing the muscles prevents the overlying skin from moving over the top of the muscle and thus decreases the appearance of the fine lines and wrinkles.2 While neurotoxins have been extensively used for various medical purposes and originally were used to treat blepharospasm and strabismus, their cosmetic applications have been in use since 1998 and can be quite effective in the periocular region.3
Understanding the Impact on Muscles is Key
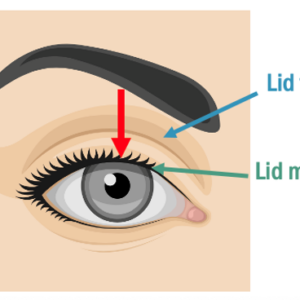
Typical injections are used in the glabella region for “frown lines,”4 in the frontalis for “forehead lines,” and the orbicularis oculi for “crow’s feet.” These are all muscles that we, as ODs, observe and understand. We understand the effects of paralyzing muscles and how that can affect the blink, can cause brow or blepharoptosis, or ultimately achieve the desired look patients are wanting without the unwanted side effects that happen when muscle movement is diminished or paralyzed.6 A prime example is the injection into the orbicularis oculi. This muscle closes the eye and is very important in maintaining the health of the ocular surface through a proper blink. If an injector gets aggressive, chasing the wrinkles in the crow’s feet area, dry eye can occur or be exacerbated because of the diminishment of the action of the orbicularis muscle. This is one of the many reasons why I believe optometrists should be performing these injections.



Neurotoxins, typically, can last anywhere from three to six months, depending on the individual. The procedure is minimally invasive and requires very little to no downtime, with full effects occurring by the end of 14 days.7 When I perform injections on new patients, it’s particularly useful to reassess their results in 14 days so that I can add more units to reach the full desired result if it wasn’t reached with the initial injections.
Treatments Can Provide a Boost of Confidence
I have found offering this service to my patients has given them more confidence and has provided more value in our relationship. I love to give my patients another reason to come see me while providing them an opportunity to not only see their best but look and feel their best. We as optometrists are already familiar with our patients’ histories and eye care needs, and we can seamlessly integrate neurotoxin treatments into our existing practices. This allows our patients to receive comprehensive care under one roof, saving them the hassle of seeking separate aesthetic procedures.
By expanding our scope of practice to include neurotoxin treatments, optometrists can provide holistic care that encompasses both vision health and periocular aesthetics. This comprehensive approach not only benefits patients but also enhances the professional growth and fulfillment of optometry as a profession. I personally love learning the science, but I very much appreciate and love the art of modifying and enhancing my patients’ appearance. In fact, adding this to my practice back in 2016 has brought me great joy. Neurotoxins have revolutionized aesthetic medicine, and their integration into optometry practices offers a transformative opportunity to address the periocular aging concerns of patients and further reinforces our expertise in a new applied way.
References
1 Carruthers, J., & Carruthers, A. (2010). Botox: cosmetic and therapeutic uses. Dermatologic clinics, 28(3), 577-589.
2 Matarasso, S. L. (2018). Neurotoxins: what’s new? Plastic and reconstructive surgery, 141(5S Advances in Facial Surgery), 27S-32S.
3 Kane, M. A. (2003). The use of botulinum toxins for treatment of facial aging. Clinics in plastic surgery, 30(4), 605-618.
4 Carruthers, J. D., Lowe, N. J., Menter, M. A., Gibson, J., & Eadie, N. (2003). Double-blind, placebo-controlled study of the safety and efficacy of botulinum toxin type A for patients with glabellar lines. Plastic and reconstructive surgery, 112(4), 1089-1098.
6 Naga, S. S., Obagi, S., & Wroblewski, K. (2016). Current understanding of the use and outcomes of botulinum neurotoxin type A in the upper face. Archives of plastic surgery, 43(2), 119-124.
7 Woodward, J. A., & Ballard, T. N. (2015). Botulinum toxin in the periocular area. Current opinion in ophthalmology, 26(5), 440-444.