December 21, 2023
“I’m worried about these wrinkles around my eyes. I’m thinking about buying this cream…”
“See this skin tag near my eye? The thing is doc, I tried removing it myself…”
“My friends tell me that it looks like I’m sleeping while I’m talking to them, anything that can help?”
Would you be surprised if I told you that all the above are conversations that I have had in my exam room with male patients? As health care providers, we sometimes unintentionally disregard the aesthetic needs of our male patients. There is a common misconception that they either do not care about the appearance of their eyes or are hesitant to discuss their concerns. This has led to a significant gap in our approach to male patients when it comes to aesthetic care. How can we bridge this gap and help all our patients feel included and comfortable enough to explore our new ocular aesthetic endeavors? How would we approach talking about aesthetics to male patients in the exam room? We can have this conversation with our male patients too!
I’m excited to share this information and to remind us, that traditionally, in advertising and media, the aesthetic conversation leans more to us females and not so much toward males. They don’t know how they could benefit or what’s possible. This is an incredible opportunity for us as optometrists. My process delivering patient education in my exam room has led to conversions, many incredible conversations, and lifelong patients.
Addressing the Needs of Male Patients
I like to take a tactful and clinical approach. I build rapport by asking questions with genuine curiosity. In my practice, I find that my male patients readily bring up concerns about their lower eyelid dermatochalasis. They have many questions for me, and I take it as an opportunity to educate them. I let them know that I work with an oculoplastic specialist to set proper expectations and offer surgical solutions. I also share if the correction they are seeking is more likely to be considered cosmetic or if it will be considered medically necessary that their medical insurance may cover. Many patients are surprised by this and excited.
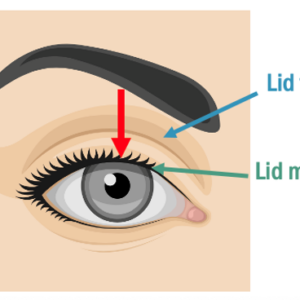
Upper eyelid dermatochalasis is a little different; my male patients don’t typically mention it without solicitation. They don’t readily recognize their upper eyelid dermatochalasis, or the significant strain it puts on their frontalis muscle and the subsequent reduction in their superior visual field. How do I broach the subject when the patient has yet to bring it up? I remind myself that it’s my duty to educate my patient about any finding that I may be recording in their chart. I say something such as, “During the exam I noticed that your eyes are closing a little more than they used to. Have you noticed this?” I proceed to take a cotton-tipped applicator and point to the exact area that I am talking about while in front of a mirror with the patient. Showing the patient this impact leads to a frank discussion. They may mention that other people around them have told them that it looks like they are not paying attention. I’ll follow up with, “This is blocking a part of your pupil and therefore blocks your vision. This unfortunately does get worse with time, but we can do something about it now, what are your thoughts?” This exchange has allowed me to refer many patients to my oculoplastic specialist, and the patients end up very happy with their results.
Low-Lying Lids Among Concerns
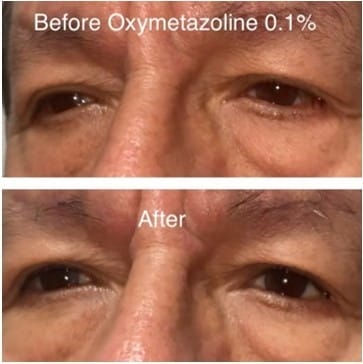
When was the last time you prescribed Upneeq to a male patient? When we learn about the male psyche, we find that they want to look energetic and address the features that make them look tired.1 Low-lying eyelids are an example of this. When evaluating for blepharoptosis, a complete eye exam with attention to extraocular muscles, pupils, and lid position is essential. I record eyelid measurements: palpebral aperture, lid crease, lagophthalmos, levator function, MRD 1, and MRD 2. For a refresher on how to take these measurements, check out “Topical Review: An Update of Diagnostic and Management Algorithms for Acquired Blepharoptosis” in Optometry and Vision Science.2
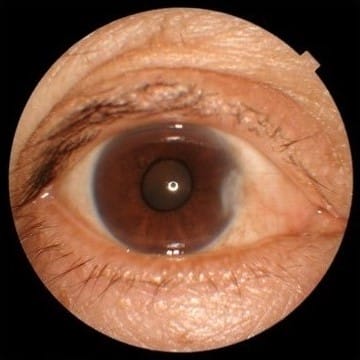
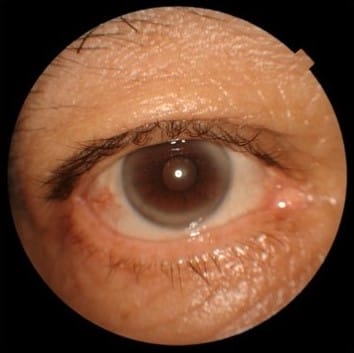
I then ask the patient if they have noticed that their eyes are tired or smaller than how they used to look. Inevitably, they will often say things such as, “Doc, that’s why I don’t send pictures to anyone anymore because my eyes look so small.” I ask them to show me older photographs of themselves to see previous eyelid positions. I also try the 2.5% phenylephrine test that I learned from Dr. Yogita Kashyap, and I add my own twist to it. I have the patient look in the mirror to remember what they look like “before,” and then I’ll instill one drop of 2.5% phenylephrine and wait two-three minutes. The phenylephrine acts on Muller’s muscle,3 the same muscle that gets activated after using oxymetazoline hydrochloride ophthalmic solution. I’ll then measure their palpebral aperture. If no other pathology is present, you can expect an elevation of 0.5mm to 1mm. I’ll then have the patient look in the mirror and ask them what they think. Once again, showing the patient and not simply telling them makes a world of a difference. I prescribe Upneeq, and my patients are excited that I gave them a solution!
Injected conjunctiva can be unsightly and a source of social discomfort in all patients, especially because other people may misinterpret this as being under the influence. As we already know, we treat the underlying cause and stabilize their ocular surface disease. We should also remember to ask, “Are you using anything else on your eyes?” They inevitably confess the use of naphazoline or a similar derivative. This is a chance to educate and redirect the patient toward recommendations that are healthy for their eyes.
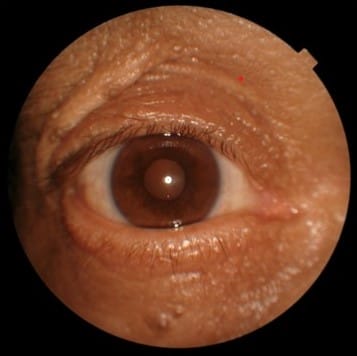
Sometimes the solutions are simpler than expected. I had a young male present to clinic for a pterygium evaluation. I asked him if he was interested in pterygium excision. He declined, so I treated the underlying dry eye symptoms. When he came back, he said to me “I feel better, but what can we do about my pterygium?” I said, “Have you thought about it some more, do you want it surgically removed?” and he replied in the negative. I then asked, “What is it that concerns you about the pterygium?” and he said, “The redness. I don’t want it to be red.” Easy fix, add on Lumify brimonidine tartrate ophthalmic solution 0.025% (Bausch + Lomb). After this encounter I now include Lumify as a part of my initial discussion of ocular surface treatments in all my patients with pterygia. To help combat overuse I recommend that patients use Lumify once a day and to give themselves a break when possible. Getting your patient to feel good is great, but if you are also giving them the added value and benefit of looking good, you’ve created a patient relationship for life.
Stress Ocular Health and Wellness
Eyelid lesions can also be problematic and bothersome to our male patients. One day I was observing a middle-aged male patient outside of the slit lamp, something we should always do, and he had what looked like a small abrasion on his temporal adnexa. I asked, “What happened here?” to which he replied, “You see this skin tag? I was trying to remove it myself with salicylic acid, but I didn’t want the acid to get too close to my eye, so I ended up missing the spot.” My curiosity allowed the patient to tell me what really happened, and this led to a referral for excision and biopsy of the lesion and a reminder to the patient to not conduct do-it-yourself eye care. In this patient scenario, I would say, “May I ask how long has this been there? Is it bothering you? If yes, here is what we can do, and if not, know that if you change your mind, it can be removed.”
This beautifully ties into other aesthetic treatments. More and more I am noticing male patients coming in for ocular surface dry eye treatments because of how it affects their appearance. The non-surgical options that we offer such as intense pulse light (IPL), radiofrequency (RF), and low-level laser (light) therapy (LLLT) are effective and are can enhance and maintain one’s appearance. I ask, “Have you thought about your facial rosacea? The redness around your eyelids?” With neurotoxin, tactfully ask, “Are there any wrinkles around your eyes like the glabellar folds or what we call the ’11s’ that bother you? We have solutions for that.”
Another helpful tip is to not make the patient self-concious or to have them develop a complex because of your approach. If you’re unsure of how the patient is taking in the new information, you can say, “My intention is to let you know about what can be done for the eye/eyelid area because I find many of my patients have questions they didn’t know I had the answers to. I want to ensure that you get all the information that pertains to the delicate eye area that I specialize in, and I want to let you know about options and solutions.” This puts most patients at ease. Framing the treatment as one of ocular health and maintaining wellness makes it that much more approachable to the male patient who may not have previously considered an aesthetic procedure.4 On a similar note, prescribe SPF products and ophthalmic sun lenses to our male patients who may not have a current skincare routine. Also, review any nutritional supplements that would benefit them.
As optometrists it is our responsibility to guide and educate all our patients through the aging process. Equipping our patients and becoming their trusted advisor is a great opportunity. Armed with knowledge on measures our patients can take during this transformative journey, we foster trust, enhance doctor-patient communication, leading to better results and happier patients for life.
Helpful Tips:
- Employ curiousity and thoughtfulness
- Show the patient instead of telling them
- Make your intentions clear
- Observe the patient outside the slit lamp
- Perform eyelid measurements
- “I noticed this about your eyes, have you?”
- “Is this bothering you?”
- “Are you using anything at all in or around your eyes?”
References
1 Fried RG. Esthetic treatment modalities in men: psychologic aspects of male cosmetic patients. Dermatol Ther. 2007 Nov-Dec;20(6):379-84. doi: 10.1111/j.1529-8019.2007.00152.x. PMID: 18093010.
2 Nichols, Kelly K. OD, MPH, PhD, FAAO1∗; Malloy, Kelly A. OD, FAAO; Karpecki, Paul M. OD, FAAO; Bacharach, Jason MD; Douglas, Raymond S. MD, PhD; Foster, Shane OD; Gromacki, Susan J. OD, MS, FAAO; Whitley, Walter O. OD, MBA, FAAO. Topical Review: An Update of Diagnostic and Management Algorithms for Acquired Blepharoptosis. Optometry and Vision Science 99(3):p 230-240, March 2022. | DOI: 10.1097/OPX.0000000000001868
3 Yom, K. H., Ricca, A. M., & Ko, A. C. (2018, July 31). Phenylephrine Response in Upper Eyelid Ptosis. Phenylephrine response in upper eyelid ptosis.
4 Farhadian JA, Bloom BS, Brauer JA. Male Aesthetics: A Review of Facial Anatomy and Pertinent Clinical Implications. J Drugs Dermatol. 2015 Sep;14(9):1029-34. PMID: 26355624.