January 19, 2024
A friend was diagnosed with open-angle glaucoma (OAG) several years ago. He was in his late 40s and had thick pachymetry values (610 um in each eye) with intraocular pressure (IOP) in the high teens, so this was not the classic glaucoma presentation. After being told he might have glaucoma, he went to a glaucoma specialist I recommended with the diagnosis confirmed. I discussed the findings with the doctor and asked why he thought glaucoma had developed without the common risks being present (age, IOP, pachymetry).1 The doctor replied that the case was not unusual as high myopia was present (approximately -8.00D in each eye). I now use this case during grand rounds presentations, and people who see a lot of glaucoma agree that myopia as a risk factor is underappreciated.
While myopia has been known to be a risk factor for glaucoma, there are reasons why it has not received the attention it deserves.2 Higher degrees of myopia are unusual and not well represented in most trials or in most clinical populations. The risk between OAG and myopia is continuous though not linear. 2,3 All degrees of myopia increase risk with a steeper degree associated with higher amounts of myopia.4
Marcus in a meta-analysis examined odds ratios for myopia as a risk factor for OAG and found a 1.35 odds ratio (OR) for low myopia (up to 3.00D), moderate myopia (-3.00D to -6.00D) with a 1.65 OR, and high myopia (>-6.00D) with a OR of 2.462. One study reported that for each diopter increase, the risk of glaucoma increases by approximately 20% and steepening with higher amounts of myopia.5
Myopia Cases on the Rise Worldwide
What makes the relationship between myopia and glaucoma concerning is that there is a global myopia epidemic with cases escalating every year.6 While the increase is greatest in Asian populations, it is occurring everywhere, including in the United States. It is estimated that by the year 2050, half of the world’s population will have myopia and 10% with high myopia.6 When one considers risk factors for the development of glaucoma, high IOP and age are at the top of the list, but myopia may join the group. The Beijing Eye Study showed the 10-year incidence of OAG to be 3.0%, which is not that different from other reports. But they found that in highly myopic populations, there was a 7.3-fold increased incidence compared to emmetropic eyes.4
Myopia and the Environment
Myopia was once thought to be genetic in origin with minor environmental influences, but recent studies have shown that environmental factors play a larger role than previously thought.7 The reasons why environmental stress is important is complex and involves more than simply reading up close. For example, time spent outdoors may have an ameliorating affect.7 An unanswered question is why those with myopia are at greater risk for developing open-angle glaucoma.8 Is it due to the development of a larger eye with stretching of tissues (peripapillary region or lamina cribosa)? Could myopic deformation of the optic nerve head be the problem? Or could it be the relationship with axial length?
OCT Evaluation Often Challenging
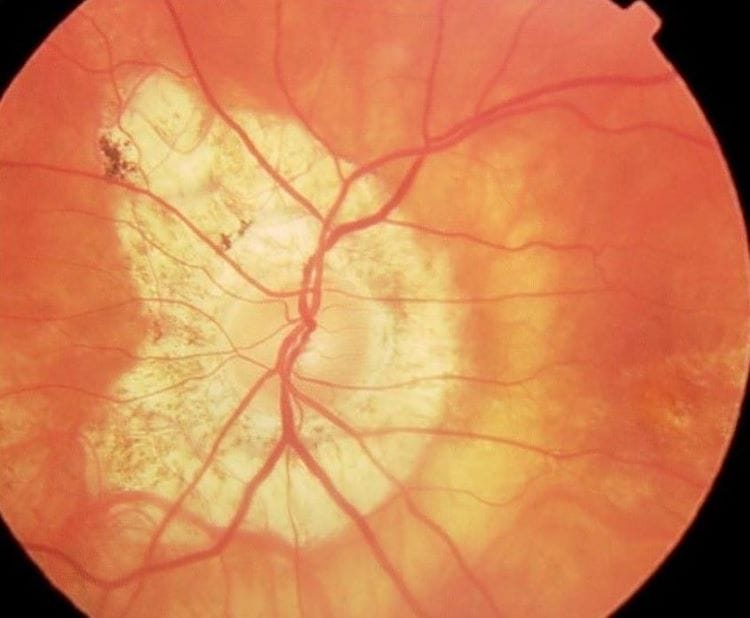
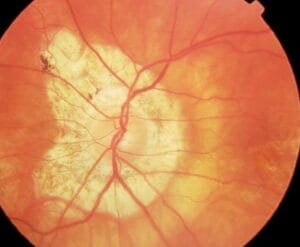
Evaluating the glaucomatous optic nerve and surrounding tissue is difficult as a myopic optic disc may mimic signs associated with glaucoma.9 For example, the myopic optic nerve often has a thin neuroretinal rim, peripapillary atrophy, and optic disc tilt.9
Even when optical coherence tomography (OCT) is used, the diagnosis is challenging as both the OCT (and perimetry) reference databases only go up to -6.00D, so larger refractive errors are not represented.10 Highly myopic patients’ scans are compared to individuals with lesser amounts of myopia, which can lead to diagnostic errors.
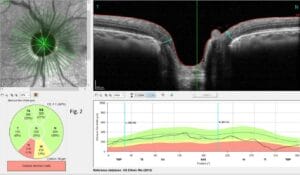
In work by Biswas, a custom myopic reference OCT database was created and showed how specificity can be improved without a loss of sensitivity.10 OCT evaluation is difficult as the basement membrane opening detection is at times elusive.11
The optic nerve torsion/rotation also makes nerve assessment difficult, which leads to inaccurate measurements.11 This explains why macula OCT scanning may be useful. More than 50% of the retinal ganglion cells are in the macula region and will show loss early.12
Myopia-related artifacts found on OCT scans are common and require careful assessment.13 One needs to evaluate the OCT scans and not just the color coding. Check for segmentation errors, location of RNFL peaks, and accuracy of basement membrane opening segmentation. And when looking at macula scans, watch for myopic maculopathies. If artifacts are found on OCT scans, one can still use the data to monitor for change over time.
Finally, some myopes have had refractive surgery with thinning of the cornea, which creates an artificially low IOP reading, reducing IOP’s role as a biomarker. In addition, there may be visual field loss in high myopia due to peripapillary atrophy and conus around the optic nerve that may occur without glaucoma being present.14
Studies have shown common genetic causes between myopia and primary open-angle glaucoma (POAG), but a causative gene has not been found.15 It appears that myopia is a causal factor for POAG, but there is also a bidirectional relationship.15 Perhaps treatment to halt myopia may also influence glaucoma risk. And there is evidence that the effect of myopia on glaucoma may be mediated by IOP, which suggests glaucoma medications are an important therapeutic tool.
There is a great deal that we do not understand about the relationship between glaucoma and myopia. When high myopia is present, the risk for the development of glaucoma is significant, which means that monitoring over time and patient education are important. Since myopia is becoming more prevalent, the numbers in both groups will continue to rise, which necessitates vigilance on our part.
References
1 Gordon MO, Beiser JA, Brandt JD,, et al The Ocular Hypertension Treatment Study; baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120 (6): 714-720.
2 Marcus MW, de Vries MM, Montollo FGJ, et al. Myopia as a risk factor for open-angle glaucoma: A systemic review and meta-analysis. Arch Ophthalmol 2011; l18 (10): 1989-1994.
3 Mitchell P, Hourihan F, Sandbach J, et al. The relationship between glaucoma and myopia. The Blue Mountains Eye Study. 1999; 106:2010-15.
4 Wang YX, Yang H, Wei CC, et al. High myopia as risk factor for the 10-year incidence of open-angle glaucoma in the Beijing Eye Study. Br J Ophthalmol 2023;107:935-940.
5 Ha A, Chung YK, Shim SR, et al. Degree of myopia and glaucoma risk: A dose-response meta-analysis. 2022 Am J Ophthalmol 236 (4); 107-119.
6 Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 to 2050. Ophthalmology 2016; 123 (5): 1036-1042.
7 Cai X-B, Shen S-R, Chen D-F, et al. An overview of myopia genetics. Exp Eye Res. 2019 Nov:188:107778. doi: 10.1016/j.exer.2019.107778. Epub 2019 Aug 28.
8 Rezapour J, Cowd C, Dohleman J, et al. Macula structural and vascular differences in glaucoma eyes with and without high axial myopia. Br J Ophthalmol 2023;107: 1286-1294.
9 Jonas JB, Wang YX, Dong L, et al. High myopia and glaucoma-like neuropathy. Asia Pacific J Ophthalmol 2020;9:234-238.
10 Biswas B, Lin C, Leung CKS. Evaluation of a myopic normative database for analysis of retinal nerve fiber layer thickness. JAMA Ophthalmol 2016; 134(9): 1032-39.
11 Zheng F, Wu Z, Leurng CKS. Detection of Bruch’s Membrane Opening in Healthy Individuals and Glaucoma Patients with and without High Myopia. Ophthalmology 2018; 125(10):1537-1546.
12 Kamalipour A, Moghimi S. Macula Optical Coherence Tomography Imaging in Glaucoma. J Ophthalmic Vis Res 2021; 16 (3): 478–489.
13 Zemborain ZZ, Jarukasetphon R, Tsamis, et al. Optical Coherence Tomography can be used to assess glaucomatous optic nerve damage in most eyes with high myopia. J of Glaucoma 2022; 29(10):833-845.
14 Ding X, Chang RT. Visual field defect classification in the Zhongshan Ophthalmic Center-Brien Holden Vision Institute High Myopia Registry Study. Brit J Ophthalmol 2016;100(12):1697-1702.
15 Chong RS, Li H, Cheong AJY, et al. Mendelian randomization implicates bidirectional association between myopia and primary open-angle glaucoma or intraocular pressure. Ophthalmology 2023;130:394-403.