November 21, 2023
“The very first step towards success in any occupation is to become interested in it.” — Dr. William Osler
Upon graduating from New England College of Optometry in 2004, I started to work as a comprehensive optometrist in private practice. In addition, I worked part time in a refractive surgery clinic at Cincinnati Eye Institute. However, patients would show up for dilated eye exams in both clinics, and often, I would see something in the retina that I just did not quite know what it was. Seeing the lesion in the retina is half the battle, the other half is knowing what it is and how to treat it. These were the days before OCT and Optos were available in clinics. (I know, I am old). My curiosity about the retina grew, and before I knew it, I landed a full-time job in the retina specialty clinic at Cincinnati Eye Institute.
Landing My Dream Job
Funny story, the retina specialist had me follow him in his clinic for a day as part of my interview, and sure enough one of my patients who I had referred from my private practice clinic showed up with a “peripheral lesion.” Suddenly, I had a lump in my throat and sweaty hands. Nerves overtook my whole body. I wanted to look smart in front of this retina specialist, but I was fearful that I didn’t really know what that “lesion” was. As he looked into the patient’s eye, he said that I had correctly diagnosed and referred this patient for a subclinical retinal detachment with a far peripheral horseshoe tear. As I followed the retina specialist into the laser suite, I was able to witness the treatment of the tear I had found. I had never felt more proud. I had quickly found the job of my dreams.
For 10 years, five days a week, and countless hours a day, I would go into the exam lane ahead of the retina specialist, take notes, draw the retina, and write the plan and assessment. (Yes, in the beginning of my retina career we were using paper, this was also before the time of electronic medical records). We would see more than 100 patients together every single day. The hours were long, but the work was so interesting that I did not mind spending the time.
The Daily Routine at My Current Practice
Fast forward to my clinic space today where I see approximately 40 to 50 retina patients a day. I work alongside 10 retina specialists and four retina fellows. We work diligently as a team to manage and treat patients from all over the world. Step inside a day in the life of an optometrist in a retina specialty practice. The days are fun, unpredictable, and most rewarding.
I arrive at clinic as my first patient of the day is starting to be worked up by the ophthalmic technician who will gather a chief complaint, visual acuity, color vision, Amsler grid testing, pupils, EOMS, IOP, blood pressure, and dilation. Next, the patient reports to the photography department for appropriate fundus imaging. Finally, the patient is seated in my exam lane.
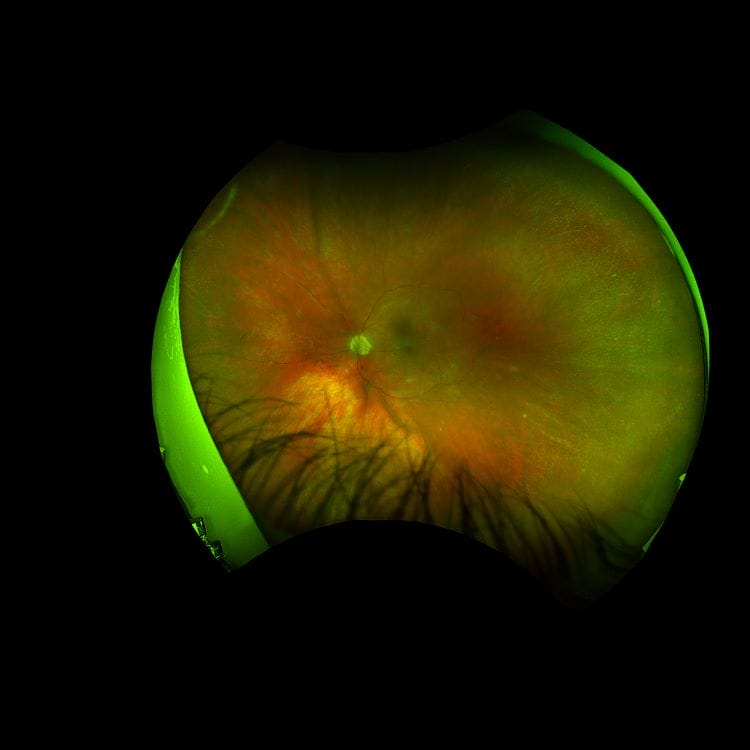
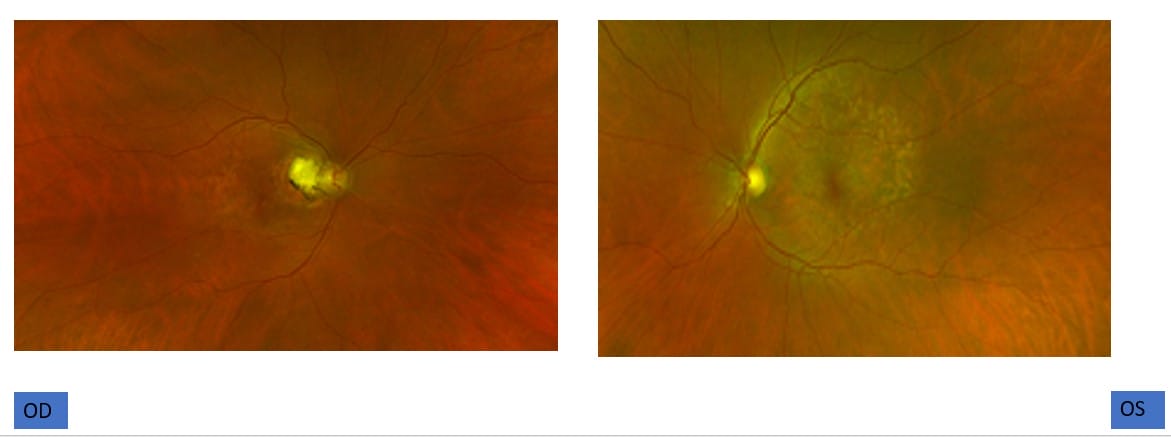
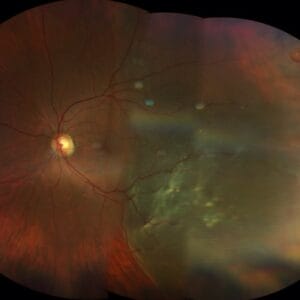
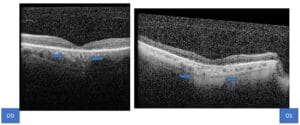
The first patient is new to my clinic and has been referred for an evaluation of age-related macular degeneration (AMD). The 87-year-old male has counting fingers vision at 2 feet in both eyes. He complains that he has had poor color vision nearly his whole life. As he grew older, his vision continued to worsen in both eyes. Amsler grid testing shows metamorphopsia in both eyes. The dilated fundus exam reveals pigmented mottling of the fundus in both eyes. This presentation is not what one would expect for age-related macular degeneration, as there were no drusen present (Figure A). The OCT shows hypertansmission defects due to a compromised RPE layer in both eyes centrally (Figure B).

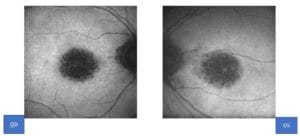
The AF reveals significant central hypoautoflourescence (Figure C). Since this does not seem like classic AMD, I asked the nurse to take a sample of blood for the Invitae Inherited Retinal Disorders genetic testing. We await the results but suspect cone dystrophy will be the diagnosis. The patient has been given an Amsler grid to monitor vision at home and is placed on AREDS2. We will call the patient with the genetic testing results and plan follow-up care once the results are received.
Distorted Vision with Worsening Depth Perception
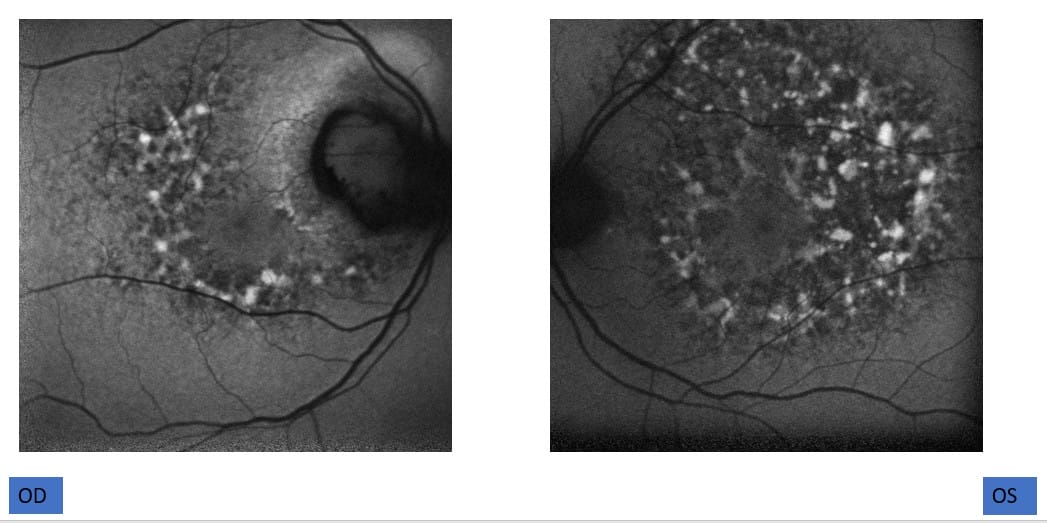
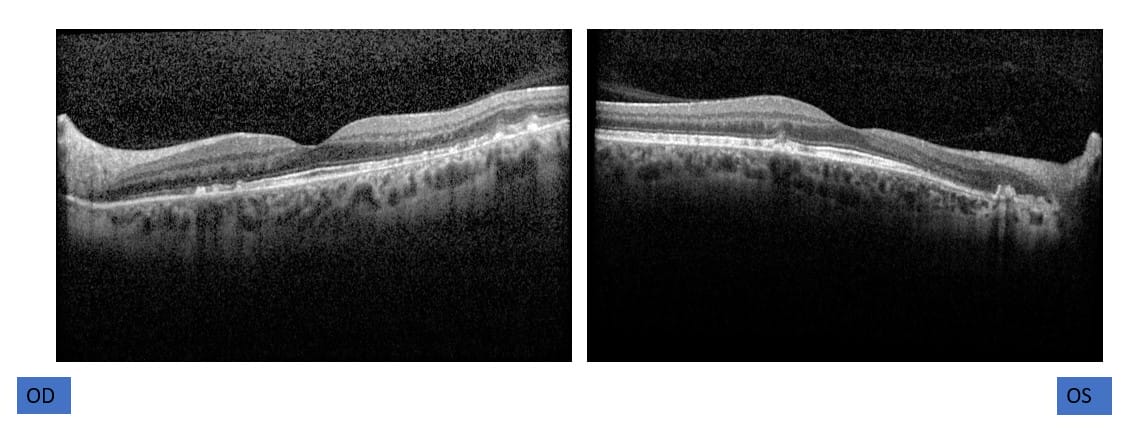
A 51-year-old female presents next. She has a history of an idiopathic parapapillary choroidal neovascular membrane that has been quiescent since diagnosis in 2017. The patient had returned to clinic in 2020 for further testing and complains of nyctalopia and headache. At that time, it was realized that the patient had been taking pentosan polysulfate sodium (PPS) for 24 years for interstitial cystitis. (The first case of PPS toxicity was not realized until 2018.) Immediately, the patient was instructed to stop the use of PPS. Today, the patient complains of distorted vision with worsening depth perception in both eyes. Visual acuities were recorded as 20/50 in the right eye and 20/80 in the left eye. Dilated fundus exam reveals toxic maculopathy consistent with history of PPS with paracentral pale yellow deposits in both eyes (old PPCNVM OD) (Figure D). The AF shows a dense array of hyper-and hypoautofluorescent spots (Figure E). Notice the foci of nodular RPE enlargement on OCT (Figure F). The patient will continue to monitor her vision at home and call for any changes in vision as a recurrent or new CNVM may occur.
There’s No Shortage of Interesting Cases
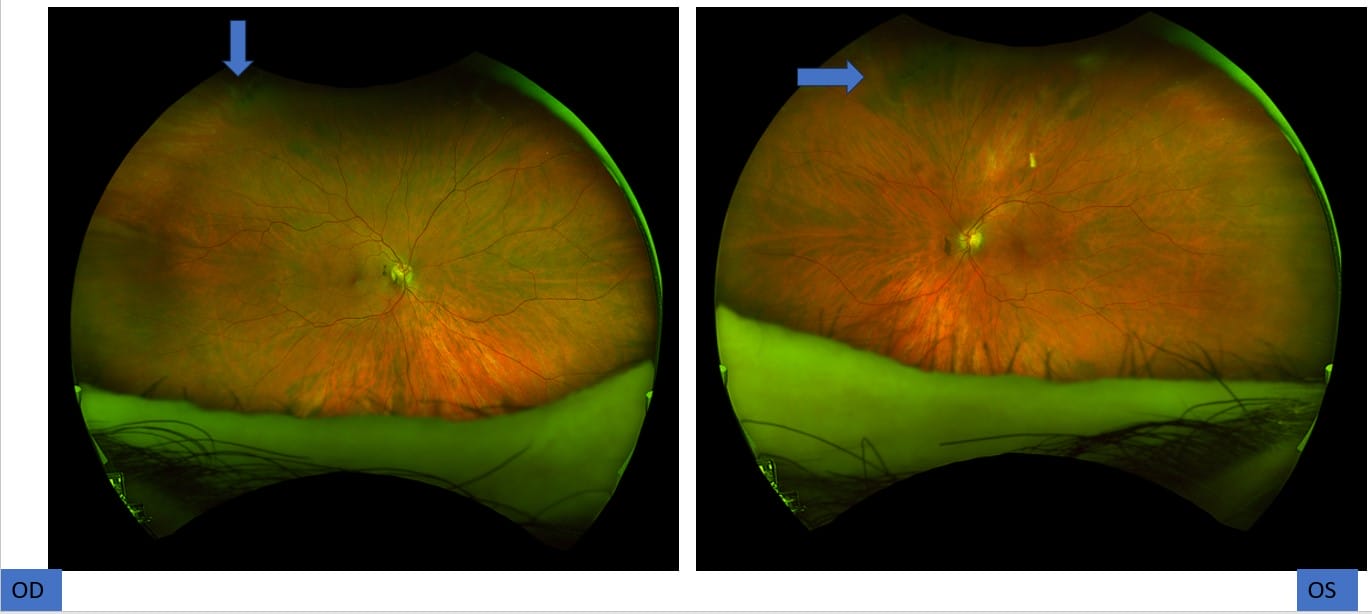
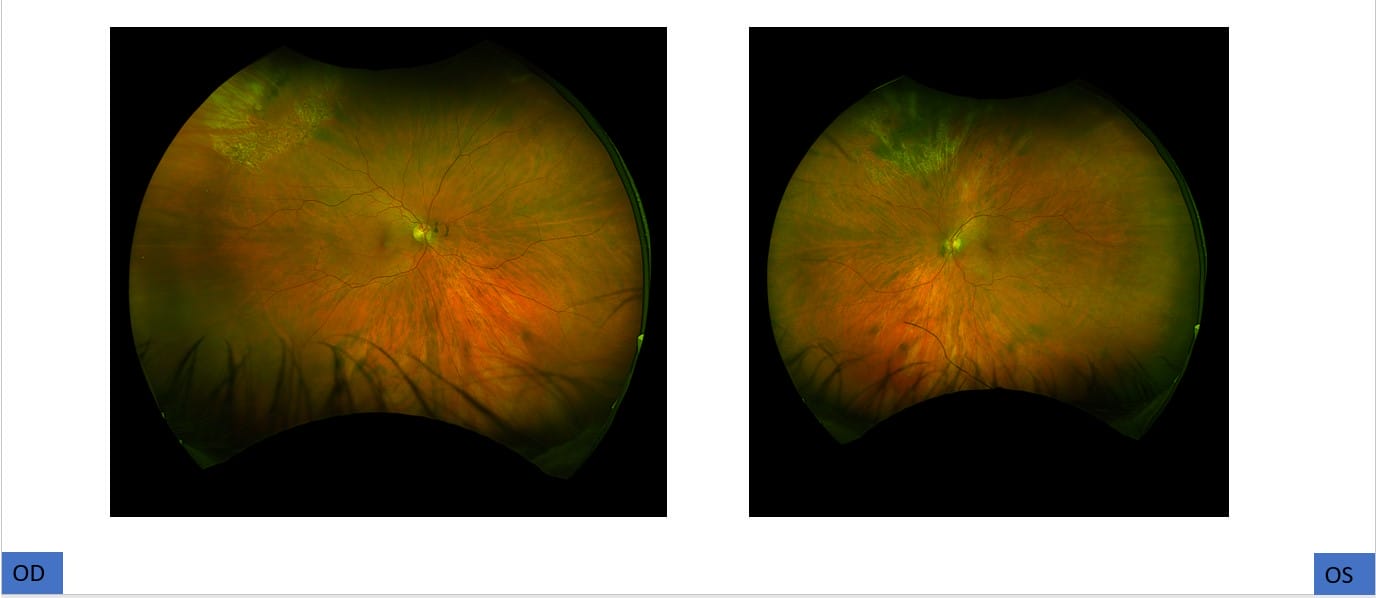
The next patient presents for a follow-up from a local optometrist’s office. The optometrist is concerned that the patient has a new retinal tear in the left eye. The chief complaint includes recent floaters and occasional flashes in both eyes for the past month. Bilateral posterior vitreous detachments were noted. A careful scleral depressed exam was performed to reveal a retinal tear along the edge of lattice degeneration in the left eye. Clinical pearl: Never forget to look at the fellow eye because often the pathology will present in the mirror image. Sure enough, there was a small retinal break that was present (barely visible on the Optos scan) in the right eye (Figure G). You can see how eye steering will help highlight the break in the left eye. The patient was treated by our office immediately with peripheral retinal laser in both eyes (Figure H).
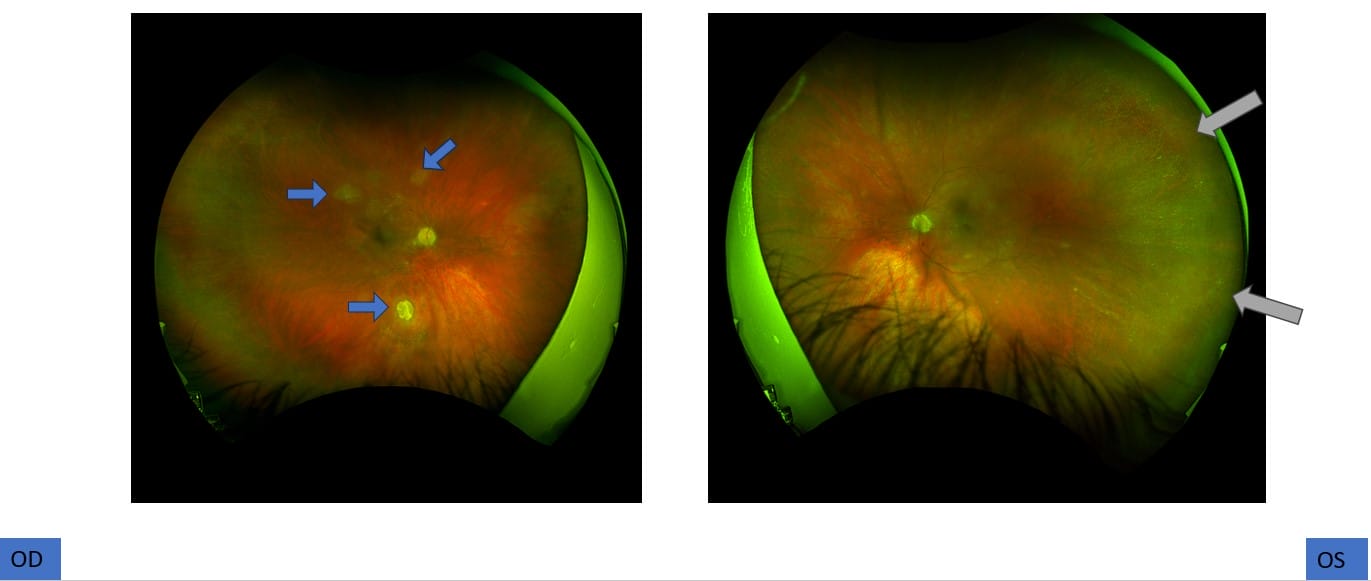
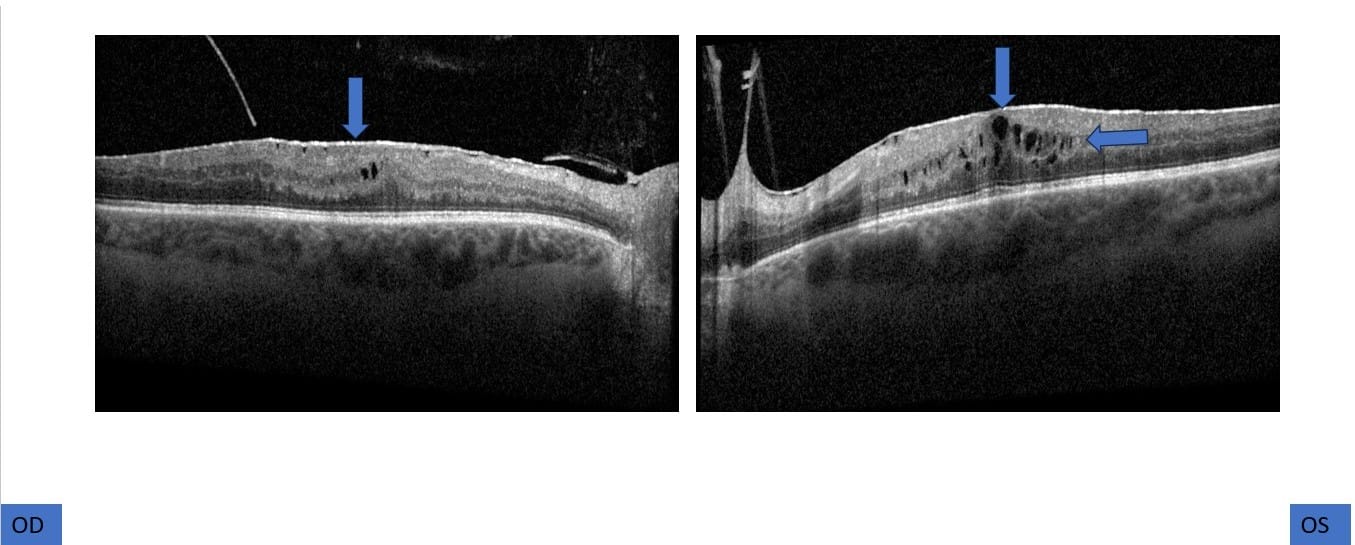
The day was busy, and several other interesting cases presented including a young gentleman with tuberous sclerosis and inactive lesions present. A retinoschisis cavity was noted temporally in the left eye (Figure I). This was a complex case that I referred to one of our retina specialists for possible pars plana vitrectomy and membrane peel due to extensive epiretinal membranes present as seen on the OCT (Figure J) in both eyes. Guarded prognosis is given to this patient, and observation may be warranted by the retina specialist as there is optic nerve atrophy in both eyes.
Other cases filled the day with our typical diabetic retinopathy, dry and wet age-related macular degeneration, presumed ocular histoplasmosis, and retinal telangiectasias.
The best way to end the day is with a patient who is forever grateful for your services. Upon entering the exam room, the patient simply pointed at the scar on his neck and said, “Thank you, Dr. Yackey. You saved my life.” A month prior, the patient had presented with an acute loss of vision in his eye. A Hollenhorst plaque was noted, a central retinal artery occlusion was diagnosed, and the patient was immediately sent to the emergency room for a stroke workup. The patient was found to have blockage in his carotid artery so dissection was performed immediately.
Needless to say, I love my interesting job as an optometrist in a retina specialty clinic.