November 2, 2023
The eyelids are getting so much love these days, so here is what you need to know as an eye care professional about how to properly assess eyelids, what can go wrong, and how we have an opportunity to make it right. Evaluating eyelids is essential to comprehensively caring for our patients.
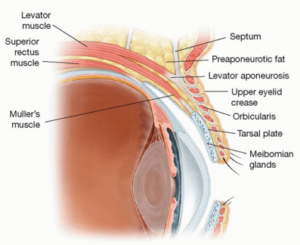
We should all already know that eyelids play a critical role in ocular surface health and maintaining visual function, and eyelashes are not just attached to the lids for adornment. They are designed to keep offenders off the front surface of the eye. The way the eyelids move, blinking spreads the tear film, pushes meibum onto the cornea, and facilitates keeping the avascular cornea bathed in more than 2,000 proteins, lipases, growth factors, and other nutrients. Before delving into the assessment, we must first understand the anatomy of the eyelids. See Figure 1.
Figure 1. The important structures that make up the eyelids.
The levator and Muller’s muscle are responsible for elevating the lid. The levator muscle is part of the levator aponeurosis complex, which functions through innervation of CNIII. When the levator is contracted, it transmits forces of this complex that inserts in the tarsal plate, lifting the eyelid. This levator aponeurosis extends from the orbital rim down to the upper border of the tarsal plant, forming the lid crease, and it fuses with the frontalis muscle superiorly, which elevates the forehead and is responsible for raising the eyebrows. This must all work in conjunction and with the help of the sympathetically innervated Muller’s muscle.
Eyelid Ptosis and What Causes It
This system can break down, resulting in ptosis through aponeurotic stretching or disinsertion of the levator muscle, which is the most common. Other causes of ptosis can be neurogenic in nature such as what we see with neurotoxin migration. Migration is usually due to poor technique or the patient rubbing the medication and physically moving it where it is not desired. Injuries can result in traumatic damage and subsequent ptosis. Mechanical problems such as excess skin seen in dermatochalasis or heaviness associated with eyelash extensions can also be a cause of ptosis. Myogenic problems such as those seen in myasthenia gravis can also be a culprit of eyelid ptosis. Once the reason is properly determined, solutions can be as simple as writing a prescription for oxymetazoline 0.1% for acquired aponeurosis, to imaging and emergency referral in the case of a third-nerve palsy or Horner’s syndrome.
Examining the Eyelid
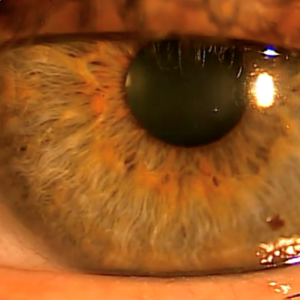
First things first, how to assess an eyelid. Look for lid position, symmetry, and lid platform. Looking for a few key identifiers won’t take up a lot of chair time and can be done while you are “chatting” with your patients. Look at where the eyelids are in relation to the iris. The lower lid should be even with the limbus without scleral showing, as seen in Figure 2. This figure also shows a great “twinkle” with the light reflections of the cornea.

Figure 2. When assessing the eyelid, the lower lid should be even with the limbus without scleral showing.
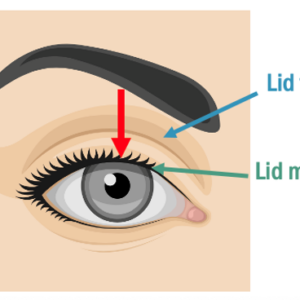
The upper lid will cover the iris, but how much is too much? A great way to look is to determine where the upper lid is in relation to the pupil. For precise measurements, use the marginal reflex distance-1 (MRD-1), as shown in Figure 3.
Figure 3. From normal MRD-1 to severely reduced MRD-1.
Normal MRD-1 should be between 4-5 mm. My favorite way to assess the lid is by looking at lid platform (Figure 4) along with observing MRD-1. (No ruler needed!)
 Figure 4. Variations in lid platform.
Figure 4. Variations in lid platform.
Normal lid platform measurements should be between 8-9 mm in men, 10-11 mm in women, and can vary by race.
Look for dermatochalasis-redundant skin that can eventually need to be surgically addressed with a blepharoplasty if it becomes visually significant or if it’s bothersome to the patient. Often patients will utilize frontalis recruitment, which is when patients utilize the frontalis muscle in their forehead to elevate or pull up their heavy brow, heavy skin, heavy lid, or sometimes all three. Imagine the amount of “eye” fatigue that occurs when that muscle is constantly engaged.
Look for Suspicious Lesions
Once we assess the patient outside the slit-lamp, it’s time to address the lids behind the slit-lamp. Examine the eyelids for lumps and bumps. Look for benign lesions such as chalazia, hordeola, verrucae, papilloma, seborrheic keratosis, cyst of moll and zeiss, sebaceous cysts, and nevi. Also be on the lookout for precursors to cancerous lesions such as actinic keratosis and keratocanthoma. Any suspicious lesion should be biopsied and can include basal cell carcinoma, squamous cell carcinoma, malignant melanoma, and sebaceous gland carcinoma. Follow your ABCDE’s (asymmetry, borders, color, diameter, and evolving). Absence of the hair follicle is another red flag. Discuss with your patients what you are looking for, and remind them that the most common place on the body to get skin cancer is, in fact, their lower eyelids. Use this opportunity to discuss the importance of sun protection with ophthalmic grade sun lenses and sunscreen.
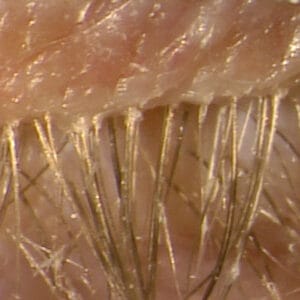
Next, have the patient look down so that the base of the eyelashes can be properly examined. The presence of collarettes is pathognomonic for demodex blepharitis. The recent approval of lotilaner 0.25% gives us the first approved medication for demodex blepharitis. It’s exciting to have a democidal treatment for this frustrating condition, and it fills an unmet need. See Figures 5A and 5B depicting one of my patients before treatment and four and a half weeks into treatment. It’s important for this patient to finish their full six-week treatment. Recall the life cycle of demodex is about 18 days, and so this will ensure the eggs are killed too.
Figure 5A (top): Before treatment with Grade 4 collarettes and demodex blepharitis.
Figure 5B (bottom): Four and a half weeks into treatment with lotilaner 0.25% BID and Grade 0 collarettes.
Explain the Risks of Lash Extensions
While you are investigating the base of the lashes, also be on the lookout for eyelash extensions and misdirected or missing lashes. If eyelash extensions are present, ensure patients properly care for them and understand the ramifications and risks that can result from wearing them. Assess and note erythema and telangiectasia, which can lead to a diagnosis of ocular rosacea. These patients also often have comorbidities alongside their rosacea such as meibomian gland dysfunction that also need to be managed. Intense pulsed light can be very effective in this patient population.
Don’t forget to pull on the lids to assess for things such as lid laxity and floppy eyelid syndrome. Floppy eyelid syndrome can have systemic ramifications, and it’s important to rule out obstructive sleep apnea-hypopnea syndrome. These conditions may require radiofrequency or surgical intervention. Lastly, push on the meibomian glands to see how many glands are functioning and what type of expression is observed, clear, cloudy, toothpaste, or none.
The eyelids give us a wealth of information and significantly contribute to the health and wellness of the ocular surface as well as contributing to the overall appearance of our patients.
It behooves us to thoroughly investigate, observe, and assess function as well as appreciate the aesthetic appearance of eyelids. Detecting abnormalities of the eyelids is part of the comprehensive exam and can lead to early intervention and better patient outcomes.
Thankfully, nothing described here requires a large time investment during the exam and can pay off in big ways for your patients. The lids deserve your attention. Their health directly impacts the overall health and look of our patients. So, get out there and show the lids and lashes some love!